News
Price-cuts for 25 medicines soon
The prices of 15 more essential medicines including neurological and diabetes drugs and life-saving intravenous antibiotics as well as 10 anti-cancer drugs are to be slashed shortly.

From left Dr. LakKumar Fernando, Dr. Kamal Jayasinghe and Prof. Asita de Silva. Pic by Amila Gamage
There can be ‘profit’ for the pharmaceutical industry but there should absolutely be no ‘profiteering’, reiterates National Medicines Regulatory Authority (NMRA) Chairman Prof. Asita de Silva in an exclusive interview with the Sunday Times on Thursday.
Profit, is financial gain, while profiteering is making or seeking to make an excessive or unfair profit.
The 25-medicine list on which will be imposed a Maximum Retail Price (MRP), will be gazetted shortly, he says, when pushed to give a date, smilingly adding that it would be “in the near future”.
With this price control, the total crucial package for diabetics including insulin, glucometers and glucometer strips, has been price-reduced, says Prof. de Silva in the two-hour interview in his office on the second floor of the NMRA down Norris Canal Road in Colombo 7. Seated with him to answer any queries were NMRA’s Chief Executive Officer Dr. Kamal Jayasinghe and Board Member and Consultant Paediatrician Dr. LakKumar Fernando.
A board on the glass-panelled wall of the Chairman’s office states: “All discussions related to product registration should be with the CEO/NMRA.” The corridors leading to the Chairman’s office are a far cry from what they were during the time of the NMRA’s predecessor, the Cosmetics, Devices and Drugs Regulatory Authority (CDDRA). Those days, the corridors and rooms of high officials were teeming with people carrying files who had come to register some product or other.
Soon after Prof. de Silva sat in the hot-seat of the NMRA, 48 medicines were price-regulated by a Gazette issued in October 2016. While most of them were from a list of 280 ‘essential’ medicines, some had been included because they were ‘widely’ used, the Sunday Times learns.
Flicking through several files to prove that whatever the NMRA has done in the past two years after he took over as Chairman has been evidence-based, he reiterates that he and his team have been engaging all stakeholders to thrash out issues and talk through what is best for the people of this country.
“It is a long process,” says Prof. de Silva, explaining that for the 25 medications currently under the microscope, verification of details including tender data, market movements etc took four long months. Thereafter, the NMRA’s Pricing Committee reviewed the list and once everything had been finalized only, that it was taken to the Health Minister.
Once the raw data are collected, the suggested list of medicines is gone through with a fine-tooth comb by the Pricing Committee headed by Dr. Palitha Abeykoon, he says, citing how one particular product was removed on the committee’s recommendations. “We follow the law to the letter.”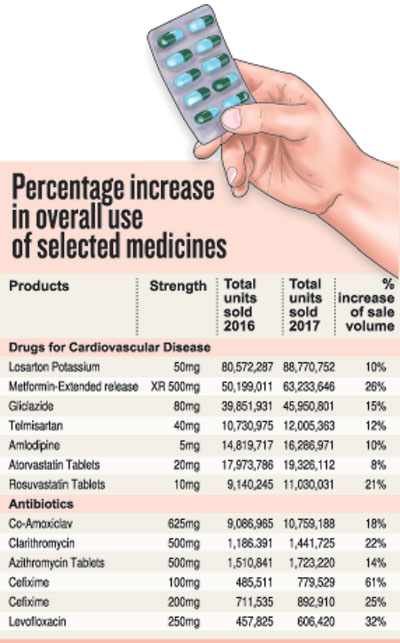
According to him the NMRA meets all the stakeholders before the drug list is gazetted. It had held discussions with the Sri Lanka Chamber of the Pharmaceutical Industry (SLCPI) on August 10.
“The NMRA works in consultation with them but not necessarily in agreement with them,” he points out.
To a query from the Sunday Times why among the 48 medicines brought under the MRP in 2016, there was no insulin (which regulates blood-sugar levels in diabetics), Prof. de Silva stressed that the price reductions were based on the market status. At that time there were only two varieties of insulin and the NMRA could not put the patients in jeopardy. However, now there are four more varieties of insulin registered, making six types available to the patients.
“We have very detailed discussions, after checking a product and before registering it. We seek a strong price commitment from the importer now,” he said.
According to Prof. de Silva who is also Senior Professor of Pharmacology of the Kelaniya University, the main difference between the earlier CDDRA and the NMRA which replaced it is that while ensuring efficacy, safety and quality, the NMRA is striving to make sure that the needs of patients are met and the cost is affordable. The main objective of the NMRA is to provide “increased access to quality-assured medicines to our patients”.
In Sri Lanka, of the funds allocated under the budget for health, 30-40% is expended on medicines. The country’s local pharmaceutical budget is a huge US$ 900 million per year. Fifty percent of it is out-of-pocket expenditure. In 2016-17, after the MRP was imposed on the 48 medicines, the saving by the patients (out-of-pocket expenditure) on brand-drug purchases was about Rs. 4.5 billion, he says, adding that “we know that the price of a medication is a key determinant of access.
Therefore, I’m mandated by law to look at pharmaceutical products”.
Looking around the world, Prof. de Silva says that all countries regulate prices of medicine except the United States of America (USA). The whole world is concerned about pricing of medicines. On September 19 and 20, there will be a regional pricing meeting of the World Health Organization (WHO) in New Delhi, India.
Referring to the United Kingdom (UK) as a leader in pharmacological economics, he says that there is profit capping with ‘incentivisation’ for pharmacies on generic substitution which means that the authorities pay an incentive to pharmacies if they dole out generics. Nearly 30% of the medicines available in the UK are generics from India. Japan, meanwhile, is the second largest market after the USA and has a National Health Insurance System under which its patients are reimbursed. A similar system is in place in Australia.
In Sri Lanka, action was needed after a damning report by a WHO expert in 2016 on unethical practices, says Prof. de Silva, asking: “So, how could we regulate pharmaceutical prices? Should they be based on CIF (cost, insurance and freight)+profit? But the CIF is not verifiable, it is loaded. Remember, even tax exemptions granted to importers are not transferred to patients. The patients have no free choice, but are guided by the prescriber (doctor) and the pharmacist who can be influenced. These two groups – the doctors and the pharmacists — have a huge amount of leverage. In an open market, pricing is stacked heavily against the patients.”
Back in 2016, the NMRA had looked at more than 450 brands, taking into account their retail market prices before gazetting the MRP for the 48 medicines. Those selling at higher prices than the MRP had to bring down their prices but those selling at lower prices were not allowed to increase them. India also started small, with 90 medicines but has now applied the MRP to over 600, he adds.
| Overall use and access to quality medicines rise, while market share of innovator brands also increases | |
| Having placed a Maximum Retail Price (MRP) on 48 medications in October 2016, the NMRA has not been resting on its laurels. A year after, in 2017, the NMRA had conducted an analysis based on IMS (International Marketing Systems) data. The analysis, according to Prof. Asita de Silva, has shown some “positive” trends: · Overall use of medicines has increased significantly indicating greater compliance with prescriptions. · Access to quality assured medicines has increased significantly, contrary to views expressed by certain groups that internationally reputed pharmaceutical manufacturers would withdraw from the Sri Lankan market. · Market shares of ‘innovator’ brands of medicine have increased rapidly, in turn making the local pharmaceutical market competitive, paving the way for a further reduction of prices. (See graphic) Pointing out that the big pharmaceutical companies too seem to have benefited by the MRP as their market share has increased, Prof. de Silva says that in the case of the patient the “increase” in the use of medicines could be due to wider usage or because more patients are taking their medications properly, whereas earlier due to high costs they may have been taking medicines only for a few days and not for the prescribed duration or on alternate days. The data indicating an overall increase in the use of medication, however, are under-estimations because they have taken into account only the retail outlets but not the private hospital pharmacies and use in private hospitals, it is understood. When looking at the trends closely, the NMRA found that people were going for innovator drugs or brands because they were now accessible at a lower cost. This has led to the big pharmaceutical companies increasing their market value, in some instances quite considerably, he said, citing the cases of lipid-lowering statins used by people with high cholesterol as well as branded paracetamol. “If you ask me whether I am happy about what the NMRA has achieved in the past two years, I will say yes. If you look at the analysis, we feel our task of providing increased access to quality assured medicines has happened,” he said, adding that no pharmaceutical company has pulled out although there was a major clamour that they would do so. There was one case of a lipid-lowering brand being withdrawn but it is back in the market now. These are the scare-mongering tactics of some interested parties. |
| How the 10 anti-cancer medicines were chosen | |
| It was a different approach for the anti-cancer medicines. Turning the spotlight on the 10 anti-cancer medications, Prof. Asita de Silva says that going by IMS data, these cost an exorbitant amount of money. Only about 10% of the cancer patients go to the private sector and buy their medications from the private sector, while the wider majority (90%), seek treatment in the state sector. As such, regulating the ‘retail’ price of anti-cancer medicines would have benefited only about 10%, according to him. “So the NMRA looked at procurement and decided that to have a bigger impact we need to regulate the tender prices, through which anti-cancer medications are being procured for the state sector,” says Prof. de Silva, getting down to numbers. “Anti-cancer medications cost the government Rs. 7.1 billion annually, of which 10 products cost about 60% or Rs. 4.2 billion. These 10, we targeted and brought down the cost to about 40%, saving the Treasury nearly Rs. 2 billion each year, which can then be used to buy more anti-cancer medications.” |
| Praise from the WHO | |
| The World Health Organization (WHO) has bestowed kudos on Sri Lanka for its action in reducing the prices of medicines.  Kusumalatha holds her monthly medicines (Picture from the WHO 2017 Annual Report) In the WHO 2017 Annual Report, under the title, ‘Making essential medicines affordable’, it has stated that “Sri Lanka’s successful regulation of pharmaceutical prices shows how evidence-based policies can protect patients’ rights, reduce OOPE (out-of-pocket expenditure), ensure affordable access to quality medicines and advance the principles of universal health coverage”. The report quotes the case of 55-year-old Kusumalatha, a diabetic who has recently been diagnosed with a heart disorder and a thyroid problem. Before October 2016, she had spent Rs. 2,000 a month for her essential medicines, but now her medicine bill is Rs. 765. Pointing out that for Kusumalatha it has made a “significant” difference, the report quotes her as saying: “If they had not reduced the prices, I would have had to give up my medicines.” Meanwhile, a WHO Country Office Report, ‘Sri Lanka’s success: Ensuring affordable essential medicines for all’, states: “The revised pricing policy is a major achievement in safeguarding patients’ rights to access affordable medicine in Sri Lanka.” |

