News
Pioneering brain surgery frees man from agonising headaches
A.K. Sarath Perera, 34, is home now, free of the excruciating headaches that have been assailing him since 2004. Originally from Dehiattakandiya in Ampara District, for now, “home” is a room in Kandy his wife, Sandamali, has rented to keep an eye on him while she has taken on the role of “rice-winner”, working as a minor employee of the Kandy Teaching Hospital.
Sarath’s headaches had been unbearable, growing in intensity and coming at all times of the day, making it impossible for him to hold down the job of a security guard. To add to his woes, his left hand had become numb and gradually useless.

Sarath on the road to recovery along with his wife Sandamali. Pic by Shane Seneviratne
As both Sarath and Sandamali take turns to talk — sometimes wracked by sobs — to me on the phone from Kandy on Tuesday (November 20), my mind flashes back to another Tuesday morning, October 30, three weeks before.
Although I feel not only a quiet excitement but some tension within me, those around me in the Neurosurgical Operating Theatre (OT) of the National Hospital in Colombo, are chatting about this and that. Like both the doctors and nurses, I too am capped and gowned, but have been told in no uncertain terms “not to touch anything and keep out of the way”, having also been barred from taking in a notebook and pen into this sterile area.
On the “table” in this state-of-the-art OT lies an anaesthetized Sarath while on the walls are a series of MRI scans, as Consultant Neurosurgeon Dr. Himashi Kularatne asks me whether I will faint on seeing blood.
Intracranial or cerebral bypass surgery — a trailblazing “first” in Sri Lanka is what I am about to witness, let alone brain surgery at close quarters, with the NHSL’s Neurosurgery team, headed by Dr. Kularatne being joined by the Plastic Surgery team headed by Consultant Plastic Surgeons Dr. Dulip Perera and Dr. Thushan Beneragama. The other important team which is part of this landmark operation is the Anaesthesia team headed by Consultant Anaesthetist Dr. Shirani Hapuarachchi.
Sarath is swathed in dark green with only a square, shaven area atop his right ear exposed to become the surgical field under the expert and skilful hands of the joint team. His head is held in place by a three-pin skull-fixation device.
Explaining that numerous are the coronary (heart) artery bypass surgeries performed in Sri Lanka, Dr. Kularatne points out that to his knowledge no cerebral bypass surgery has ever been done here before.
Having suffered since 2004 and sought treatment from many doctors including ayurveda practitioners, it had been Kandy Consultant Neurologist, Dr. Indunil Wijeweera, who had told Sarath this year that there was a block in a vessel taking blood to the brain and he would have to undergo surgery. It was then that Sarath was referred to NHSL’s Consultant Vascular Surgeon, Dr. Daminda Rajamanthri. Having been seen by Dr. Rajamanthri and also Consultant Neurologist Dr. Padma Gunaratne, Sarath had been referred to Dr. Himashi Kularatne.
The diagnosis was clear, says Dr. Kularatne, explaining that Sarath was suffering from Moyamoya disease.
With the Japanese being the first to call this condition, “moyamoya” which means “puff of smoke”, he describes the disease as a chronic and progressive narrowing of the internal carotid arteries (ICA) at the base of the brain as well as the narrowing of blood vessels inside the brain. As the artery walls become thicker, with even a complete blockage occurring, multiple strokes or haemorrhages follow.
The brain being the powerful organ that it is, the Sunday Times learns that it will not give up the fight to get oxygen-rich blood to areas which have been deprived by such thickening of the ICA. In a reaction to this threat, the brain will create tiny “collateral” or parallel blood vessels which have a hazy, filmy appearance in an angiogram.
These tiny and fragile collateral vessels which the Japanese likened to a “puff of smoke” can rupture, causing a bleed into the brain, says Dr. Kularatne reiterating the dangers. Another threat is aneurysms. With a major stroke or bleed likely to leave the patient severely disabled or paralysed, urgent treatment is essential.
The symptoms that Sarath was manifesting not only included headaches, but also numbness in the left arm and fits or seizures which were pointers to strokes, according to Dr. Kularatne, who adds that the cause of moyamoya disease is unknown but heredity seems to be an explanation.
In the OT, the neuro-and-plastic joint team is about to create a new pathway for blood to be carried to Sarath’s brain. This is called re-vascularization. As his exposed scalp is prepped with antiseptic, the discussion among the team revolves around Plan A and B, for re-vascularization can be direct or indirect.
Plan A or direct re-vascularization, the Sunday Times learns, is a “vessel graft” in which the superficial temporal artery (STA) from outside the brain is connected to the middle cerebral artery (MCA) inside the brain, bypassing the narrowed or blocked ICA and re-routing the blood flow.
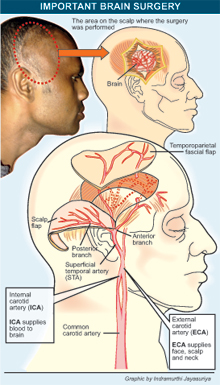
Plan B or indirect re-vascularization involves muscle flaps. Here the temporalis muscle on the side of the head as well as the temporoparietal fascia with the STA are dissected and placed adjoining each other on the surface of the brain affected by the ICA block. This will result in new blood vessels forming between the blood-rich muscle and fascia and the brain, explains Dr. Beneragama, calling the procedure by the jaw-breaker of ‘encephalo-myo-fascio-synangiosis’.
Before making the incision on Sarath’s scalp, the STA is marked and both the temporalis muscle and the fascial flap raised separately and meticulously dissected from the underlying muscles by Dr. Perera and Dr. Beneragama. The muscles are then folded back, exposing the skull.
As I watch, the next action is the drilling of small holes in the skull to allow the sawing out of a “window” into the bone shielding the brain. In this procedure called a craniotomy, a piece of bone is removed and Dr. Kularatne steps in to gently open out the covering (dura) of the brain which is folded back, giving us the first fascinating glimpse of Sarath’s brain.
There follows a discussion and peering at the brain through a special microscope. I too get a quick peek. It is then that Dr. Kularatne, Dr. Perera and Dr. Beneragama decide that Plan A or direct re-vascularization is not possible as the thickening of the ICA is spread along quite a length. So Plan B or indirect re-vascularization it is.
“The two muscle and fascial flaps are placed side by side because a large section of Sarath’s ICA is narrowed, even inside the brain,” explains Dr. Beneragama, adding that whereas one flap would enhance the blood supply to the brain, a second would further strengthen the supply.
Nearly six hours after, having watched groundbreaking brain surgery, I leave the freezing OT around 2.30 in the afternoon, not only physically fatigued but also mentally weary, marvelling at the stamina of the team which has handled the “wonder” that is the human brain, a nick of which would end in disastrous consequences.
More than three weeks on, Sarath is doing fine. “Godak hondai,” is Sandamali’s verdict, explaining that he is much better now.
Sarath, meanwhile, overcome by emotion can only whisper that for the team which pulled him back from the brink of major disability and his wife who stood by him through thick and thin, “Budu bavath wewa”.
Tough times for family: Please help
For father, mother and daughter, it is tough times ahead. Having cleared the hurdle of a major illness in the form of Moyamoya disease, they are grappling with poverty, what with Sarath having to take 10 varieties of tablets daily and other expenses.
“My mother is looking after our daughter in Dehiattakandiya and we have to send her some money as she doesn’t have a source of income,” says Sandamali on whose shoulders is the burden of making ends meet, while also forking out Rs. 5,000 as their monthly rent for the room in Kandy.
“I need to keep Sarath close to the hospital where I work because I attend to his needs including bathing him,” she says, anxious over the mounting bills.
The doctors have given hope to this family. Generous donors, however, could ease the family’s impoverishment by sending their mite to Account No. 253-2-001-1-00-20139 at the People’s Bank branch at Aralaganwila in the name of J.M. Anoma Sandamali.
Follow @timesonlinelk
comments powered by Disqus



















