‘I was sure I would die’
The odds were against her. The risk of death on the operating table was more than 50%. A few months before, life had been usual for this pretty, slim 28-year-old living at Dehiwela. She was working at a private company while also studying for her external degree, attending lectures over the weekend.
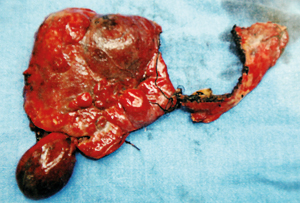
The resected haemangioma
It was for wheezing, quite common among people in Sri Lanka now, that Amila* sought treatment from Consultant Physician Dr. Chandana Amerasinghe who on examining her chest noticed a slight swelling of the liver and ordered a scan.
It was in July last year that Consultant Radiologists Dr. Nirmala Wijesinghe and Dr. Sanjeewa Munasinghe carried out the scan and yes, the liver was enlarged but Amila was perfectly normal.
Her life changed gradually — slowly but surely, the swelling increased with the liver-area becoming tender and painful. There was pressure in that area too, says Amila, explaining that “it would come and go. The pressure was not a permanent symptom, there only if I sat for a long while”.
September last year saw Amila in hospital under the care of Dr. Amerasinghe, with suspicions of cancer, making a liver biopsy under local anaesthesia a necessity.
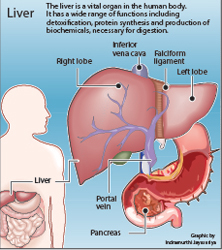
The biopsy also by Dr. Wijesinghe brought forth both good and bad news – it was not cancer, but a “complex giant liver lesion” or humongous haemangioma. It had encompassed the whole right lobe and spread to part of the left lobe of Amila’s liver.
A lesion is an abnormality or damage to tissue of an organ, MediScene understands.
“I was mentally down,” concedes Amila, reliving the agony of those days. “I was sure that I would die.”
It was then that she went to Consultant Hepatologist Prof. Janaka de Silva who immediately ordered a CT scan with a report from Dr. Sanjeewa Munasinghe.
Confirming that it was a haemangioma, the first sliver of hope was offered to Amila.“We’ll do it,” she was assured and in turn directed to Consultant Surgeon Dr. Chandika Liyanage.
By that time Amila’s life had changed drastically. The swelling was big, she found it difficult to walk and she grew tired easily. This compelled her not only to give up her studies but also her job. Giving her moral support and urging her not to be scared, the reassurances came from Dr. Liyanage that if it was impossible to remove the haemangioma, “we’ll give you a new liver”.
This was a life-changing moment for her, because she felt that she had been given a second life, she says, with tears welling up in her eyes even now as she recalls those words. Numerous tests followed, with Dr. Liyanage asking for a week’s time to let her know what the situation was. A week later, however, the picture was grim. All senior liver surgeons had discussed her case in detail.
There was a “big risk” with the chances of death on the operating table being over 50%, he told her laying bare the details.
Ordering another CT scan, Dr. Liyanage next took Amila’s case before the world. Armed with a CD of her condition, he had discussed her case with international experts when he met them at conferences in Switzerland, India and Hong Kong.
The prognosis was not good. Wait until the very last, many experts advised Dr. Liyanage, and then go in for the last resort which was a transplant with a liver from a cadaver.
Amila’s widowed mother and sister were in tears, their home in mourning. Dr. Liyanage, however, was not convinced that a liver transplant was the answer. “It will be good if we can retain your liver by resecting the diseased areas and allowing the remaining portion to re-grow, rather than performing a transplantation,” he told her.
What was the guarantee that if a liver from a brain-dead person became available, she would be the first recipient? She would have to get on the waiting list and hope for the best but time was running out, she felt.
It was family conference time for Amila because it would be her decision whether she would await a liver or allow the doctors to cut out the haemangioma and keep the little part of the liver that was not affected. The family also debated the possibility of getting it done abroad, as such an operation had not been attempted in Sri Lanka before. “The decision was to keep my liver,” she says, adding that it was the consensus among her immediate family. “I came to accept the possibility that I may die during the operation but I preferred it to be under the hands of a local doctor.”
As government hospitals did not have the facilities for such major surgery, she would have to enter Nawaloka Hospital and her family then embarked on a venture to collect the funds needed. “It was a very difficult time for me,” concedes Amila, who had been caught up between the fear of death and the hope of recovery, when most of her time she spent in meditation.
The illness too had advanced and she was in much agony and discomfort. “There was massive pressure on that side,” she recalls.
The first week of February this year, her condition began to deteriorate. Admitted to Ward 3C of the Nawaloka Hospital, the nursing team headed by Sr. Dinesha was by her side, giving her strength to face the operation.
She saw as a good omen the fact that a monk who was in hospital at the same time coming to her bedside and tying pirith nool which gave her solace and comfort.
Having undergone a battery of tests, it was Consultant Surgeon Dr. Rohan Siriwardhana who explained the complexity of the surgery, while Consultant Anaesthetist Dr. Bhagya Gunathilaka, who had the onerous task of seeing to her vital signs during the operation, pointed out that “it was a big challenge” but they would get through.
From the crack of dawn, 4 o’clock, on February 12 she had to fast and she remembers with much emotion how when she wanted thambili as her last drink, Sr. Dinesha insisted that the staff get her one, even though the hospital kitchen did not have it.
“I was not frightened while being wheeled to the operating theatre,” says Amila, but on entering the OT and seeing the gowned and masked doctors, a cold hand did grip her heart. It was then that Dr. Gunathilaka told her that Dr. Liyanage wanted to talk to her. The last words before she slipped into anaesthesia-induced unconsciousness were Dr. Liyanage’s “Baya wenna epa, api ikmanata hamu wemu”. (Do not be afraid, we will meet soon)
The four days at the Surgical Intensive Care Unit that followed the 15-hour major surgery are a daze. But soon she was back in the recovery room where her beloved mother could keep vigil by her side.
Having been in hospital from February 9-19, Amila does acknowledge that she was in a “lot of pain” but bore it up. The cut is the shape of the Mercedes Benz symbol, like a ‘Y’ turned upside down, she smiles.
With confirmation that her liver is growing, Amila is content to occupy herself at home by writing story books both in Sinhala and English for children.
Hodatama hondai, Amila says, explaining that she is very well now. She can eat anything and she is not on any medication. What is left is for her to plan her future.
The life-saving operation
This is probably the biggest and most challenging liver resection performed in Sri Lanka, says Hepatobiliary Surgeon Dr. Chandika Liyanage, giving credit for its success to the perfect coordination by the close-knit liver team of the North Colombo Teaching Hospital.
“The dilemma faced by the surgical team was to resect (remove) the tumour while leaving behind an adequate part of the liver for her survival,” Dr. Liyanage told MediScene.
A tangle of blood vessels, a liver or hepatic haemangioma is a non-malignant (non-cancerous) or benign mass in the liver, believed to be congenital.
In the case of Amila, the haemangioma or lesion which had replaced the whole of the right liver and extended to the left lobe as well, had anatomically distorted the inferior vena cava (IVC), the portal vein and the pancreas.The complex 15-hour operation on February 12, this year, was undertaken by the surgical team comprising Hepatobiliary Surgeons Dr. Liyanage and Dr. Rohan Siriwardhana; Consultant Surgeon Dr. Sumudu Kumarage; Consultant Anaesthetist Dr. Bhagya Gunathilaka; and supported by Consultant Hepatologist Prof. Janaka de Silva.
They had resected six of the eight liver segments, with careful preservation of the biliary system with intra-operative cholangiography (imaging of the bile-duct during surgery) guidance.The IVC is the large vein ascending through the abdomen which collects blood drained from the hepatic (liver) veins, the renal (kidney) veins and the phrenic (diaphragm) veins. The portal vein is the vein through which oxygen-depleted blood from the stomach, intestines, spleen, gallbladder and pancreas flows to the liver, MediScene learns.
(*Name changed to keep her identity confidential)
Follow @timesonlinelk
comments powered by Disqus
























