Dealing with Diverticular disease
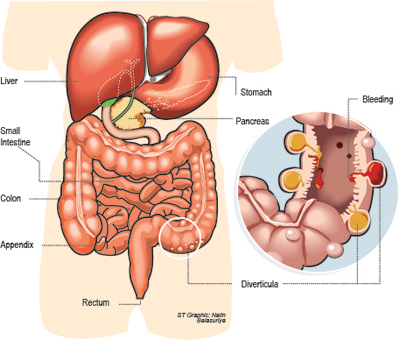
A diverticulum is a pouch-like area that can form in the muscular wall of the colon, particularly at points where blood vessels enter. Diverticular disease is a term used to describe people with diverticulosis, which causes no symptoms, and diverticulitis, which usually causes pain, nausea, vomiting, and diarrhoea.
Diverticular disease is a common problem that affects men and women equally. The risk of disease increases with age. It occurs throughout the world but is seen more commonly in developed countries.
What is Diverticular disease?
A person with diverticular disease may have diverticulosis, diverticulitis, or diverticular bleeding.
Diverticulosis - Diverticulosis is often found with a test done for other reasons, such as flexible sigmoidoscopy, colonoscopy, or barium enema.
Most people with diverticulosis have no symptoms and will remain symptom free for the rest of their lives.
Diverticulitis- Inflammation of a diverticulum (diverticulitis) occurs when there is thinning of the diverticular wall. This may be caused by increased pressure within the colon or hardened particles of stool, which can become lodged within the diverticulum. These events could decrease blood flow to the diverticulum.
The symptoms of diverticulitis depend upon the degree of inflammation present. The most common symptom is pain in the left lower abdomen. Other symptoms can include nausea and vomiting, constipation, diarrhoea, and urinary symptoms.
Diverticulitis is divided into simple and complicated forms.
Simple diverticulitis, which accounts for 75 percent of cases, is not associated with complications and typically responds to medical treatment without surgery. Complicated diverticulitis occurs in 25 percent of cases and usually requires surgery. Complications associated with diverticulitis can include the following:
Abscess – a localised collection of pus.
Fistula – an abnormal tract between two areas that are not normally connected (eg, bowel and bladder)
Obstruction – a blockage of the colon.
Peritonitis – infection involving the space around the abdominal organs.
Sepsis – overwhelming body wide infection that can lead to failure of multiple organs.
Diverticular bleeding - Diverticular bleeding occurs when a small artery located within the diverticulum breaks through into the colon.
Diverticular bleeding usually causes painless bleeding from the rectum. In about 50 percent of cases, the person will see maroon or bright red blood with bowel movements.
Is bleeding with a bowel movement normal? - It is not normal to see blood in a bowel movement; this can be a sign of several conditions, some of which are serious and require immediate treatment. Anyone who sees blood after a bowel movement should consult their doctor to determine if further testing or evaluation are needed.
Diagnosis - Diverticulosis is often found during tests performed for other reasons. The following are tests that may be recommended to diagnose diverticulosis:
Barium enema - This is an x-ray study that uses barium in an enema to view the outline of the lower intestinal tract.
Flexible sigmoidoscopy — This is an examination of the inside of the sigmoid colon with a thin, flexible tube that contains a camera.
Colonoscopy — This is an examination of the inside of the entire colon.
CT scan with insertion of contrast dye through the rectum — often used to diagnose diverticulitis and its complications.
Treatment
Diverticulosis - People with diverticulosis who do not have symptoms do not require treatment. However, most clinicians recommend increasing fibre in the diet, which can help to bulk the stools and possibly prevent the development of new diverticula, diverticulitis, or diverticular bleeding.
Fruits and vegetables are a good source of fibre. The fibre content of packaged foods can be calculated by reading the nutrition label.
Diverticulitis - Treatment of diverticulitis depends upon how severe your symptoms are.Home treatment- If you have mild symptoms of diverticulitis (mild abdominal pain, usually right lower abdomen), you can be treated at home with a clear liquid diet and oral antibiotics.
However, if you develop one or more of the following signs or symptoms, you should seek immediate medical attention:
- Temperature >100.1ºF (38ºC)
- Worsening or severe abdominal pain
- An inability to tolerate fluids
Hospital treatment - If you have moderate to severe symptoms, you may be hospitalised for treatment. During this time, you are not allowed to eat or drink; antibiotics and fluids are given into a vein.If you develop an abscess or blockage of the colon, you may require drainage of the abscess (usually performed by placing a drainage tube through the abdomen or rectum) or by surgically opening the affected area.
Surgery - If you develop a generalised infection in the abdomen (peritonitis), you will usually require emergency surgery. A two-part surgery may be necessary in some cases.
The first surgery involves removal of the diseased colon and creation of a colostomy. A colostomy is an opening between the colon and the skin, where a bag is attached to collect waste from the intestine. The lower end of the colon is temporarily sewed closed to allow it to heal. Approximately three months later, a second surgery is performed to reconnect the two parts of the colon and close the opening in the skin. You are then able to empty your bowels through the rectum.
In non-emergency situations, the diseased area of the colon can be removed and the two ends of the colon can be reconnected in one surgery, without the need for a colostomy.
Surgery versus medical therapy - Surgery to remove the diseased area of the colon may not be necessary if you improve with medical therapy. Surgery may be recommended for people with repeated attacks of diverticulitis or if there are severe or repeated episodes of bleeding. The decision depends in part upon your other medical conditions and ability to undergo general anaesthesia and surgery.
Some clinicians recommend surgery after the first attack of diverticulitis in people who are less than 40 to 50 years. The reason for this is that the disease may be more severe in this age group and there may be an increased risk of recurrent disease that will ultimately require surgery. Thus, having surgery at a young age could potentially eliminate the chances of developing worsened disease. The decision to undergo surgery ultimately depends upon your preferences.
In many cases, an elective operation can be performed laparoscopically, using small incisions, rather than the typical vertical (up and down) abdominal incision. Laparoscopic surgery usually allows you to recover faster and avoids a longer hospital stay.
After diverticulitis resolves - After an episode of diverticulitis resolves, the entire length of the colon should be evaluated to determine the extent of disease and to rule out the presence of abnormal lesions such as polyps or cancer. Recommended tests include colonoscopy, barium enema and sigmoidoscopy, or CT colonography.
Diverticular bleeding - Most cases of diverticular bleeding resolve on their own. However, some people will need further testing or treatment to stop bleeding, which may include a colonoscopy, angiography (a treatment that blocks off the bleeding artery), or surgery.
Prognosis
Diverticulosis - Over time, diverticulosis may cause no problems or it may cause episodes of bleeding and/or diverticulitis. About 15 to 25 percent of people with diverticulosis will develop diverticulitis while 5 to 15 percent will develop diverticular bleeding.
Diverticulitis - About 85 percent of people with uncomplicated diverticulitis will respond to medical treatment while about 15 percent of patients will need surgery.
After successful treatment for a first attack of diverticulitis, one-third of patients will remain asymptomatic, one-third will have episodic cramps without diverticulitis, and one-third will go on to have a second attack of diverticulitis.
The prognosis is worse following a second attack of diverticulitis; the rate of complications in this group is close to 60 percent. Only 10 percent of people remain symptom free after a second attack.
(The writer is a Consultant Physician)
Follow @timesonlinelk
comments powered by Disqus























