News
Alcohol spells socio-economic doom; national policy to make Lanka booze-free nation

The panel of the First Session on ‘Global and regional aspects and costs of alcohol’ during the National Alcohol Summit at the BMICH on Thursday. The Chairpersons Prof. Narada Warnasuriya (Chairman of SLMA’s Expert Committee on Tobacco and Alcohol) and Dr. Sudarshini Fernandopulle (Member of Parliament) are flanked (from the left) by Dag Rekve (Technical Officer, Department of Mental Health & Substance Abuse, WHO Headquarters); Dr. Nazneen Anwar (Regional Advisor on Mental Health, WHO/SEARO), Dr. Chithramalee de Silva and Dr. Nadeeka Chandraratne. A large NATA banner on the benefits of being alcohol and tobacco free. Pix by M.A. Pushpa Kumara & graphic by Nalin Balasuriya
It is a sight that greets many as the evening shadows lengthen into night — swaying, lurching and staggering, an inebriated person with obscenities spewing forth, attempting to make his way home.
Often whatever time this husband and father reaches home, the family lives in fear of what accompanies his arrival……usually the children crouch in terror in a corner of their home, while being mute witnesses of the battering and abuse directed at their mother.
Alcohol is the culprit.
It was a strong case of the ‘glass running over’ as facts and figures were poured out against alcohol, to a packed audience on Thursday, with the launch of Sri Lanka’s National Policy on Alcohol Control.
The ‘National Alcohol Summit’ at the BMICH not only heard Health Minister Rajitha Senaratne holding alcohol up for review but also Health Services Director-General Palitha Mahipala, introducing the National Policy on Alcohol Control, the initial steps towards making Sri Lanka alcohol-free.
Sending out a clear call to take immediate steps to phase out all corporate social responsibility (CSR) projects by the alcohol industry and halt the interactions of government officials with the alcohol industry, Dr. Chithramalee de Silva, the Health Ministry’s Director of Mental Health and Consultant Community Physician, built-up powerful evidence against alcohol.
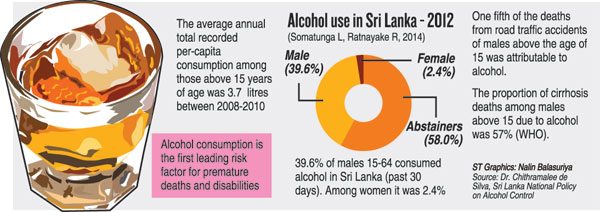
“Alcohol consumption is the first leading risk factor for premature deaths and disabilities,” she stressed, stating that alcohol is strongly linked to poverty, the high suicide rate and deliberate self-harm and gender-based violence.
Alcohol-use is a major obstacle to human development and achieving the Sustainable Development Goals set out by the United Nations, she said.
Explaining that the Health Ministry and the National Authority on Tobacco and Alcohol (NATA) took into consideration the input of all stakeholders, Dr. de Silva spelt out the priority areas of the National Policy as marketing; pricing and trade; limiting availability and accessibility; drinking and driving; community actions and surveillance, monitoring, evaluation and research.
In a nutshell, according to Dr. de Silva, this is how these priority areas will be handled:
Marketing – by eliminating all direct and indirect forms of alcohol advertising, promotion and marketing. New legislation to be drafted to cover advertising; promotions through television/cinema; and labelling and packaging of alcohol products.
Pricing, trade and investment – minimise consumption of alcohol through pricing, trade and investment policies by bringing in a mechanism for tax control and paying attention to trade agreements etc.
Availability and accessibility of alcohol products from any source — minimise the access of all types of alcohol products to those below the age of 21; prohibiting the subsidising of alcohol purchase through any means (eg. as a part of the price of an entrance ticket); prohibiting the sale of alcohol products in public gatherings where children have access (eg. sports events); and establishing a new transparent system of obtaining licences for sale of all types of alcoholic beverages.
Establish a mechanism to control illicit alcohol products — strengthen actions of Police and Excise Departments; increase measures to deter illegal production, transport and sale; and strengthen community leadership to eliminate production, distribution and sale of illicit brew.
Protect all segments of the population from the consequences of alcohol use – prohibit by law the consumption of alcohol in public places; discontinue the serving of alcohol products at public and government functions and events using public funds; eliminate disorderly conduct following alcohol use in public areas and workplaces.
Drink-driving – eliminate the driving of vehicles, road use and operation of machinery after alcohol consumption.
Passionately, she requested adequate financing as well as the implementation and monitoring of the Alcohol Policy by the Health Ministry and NATA with the active participation of all relevant sectors, to work towards an alcohol-free Sri Lanka.
Among those present at the inauguration of the summit were Health Ministry Secretary Anura Jayawickrama and World Health Organisation (WHO)’s Sri Lanka Representative Dr. Jacob Kumaresan.
| Alcohol gulps down billions of rupees in health cost The costs to the health sector due to alcohol-use last year (2015) were a huge Rs. 141.1 billion (US$ 973 million)! This ‘total cost’ which takes into account only cancer and non-communicable diseases (NCDs) can be broken down as ‘direct cost’ amounting to Rs. 35.1 billion and ‘indirect cost’ amounting to Rs. 105.8, Dr. Nadeeka Chandraratne of the Sri Lanka Medical Association said, drawing attention to the ‘Social and economic costs of alcohol in Sri Lanka’. She explained that the ‘direct cost’ includes inpatient care (hospital and treatment costs) and clinic care costs. The treatment costs include drugs, investigations, surgery, therapy such as radiation and chemotherapy etc and wound dressing etc. The ‘indirect cost’, meanwhile, includes costs due to premature mortality (death) and absenteeism (patient-inpatient days and bystander-patient admitted days). Of the Rs. 141.1 billion, the cancer costs amounted to Rs. 9.8 billion and NCDs to Rs. 131.3 billion. However, Dr. Chandraratne pointed out that these costs did not include many other costs including private sector costs; domestic violence and child abuse; legal, insurance and law-enforcement costs; Health Ministry administrative costs; and prevention and rehabilitation costs. All diseases linked to alcohol-use had also not been covered. No costing is possible with regard to the mental health burden on women and children in homes where the men are alcoholics. |

