Antibiotics causing an infection? It sounds rather ridiculous - an oxymoron of medical proportions perhaps? Yet, it is true. Antibiotics, those wondrous weapons that brazenly beat back beastly bacteria are themselves capable of causing an infection. The infection takes the form of diarrhoea.
So how can this happen? Well, it is easy to forget that, even though we take an antibiotic for an anatomically localized infection such as an infected leg or sinusitis, the antibiotic itself will be sent all over the body. This includes the bowel. It may surprise one to learn that the human bowel is the model for multiculturalism for which cosmopolitan cities like New York and London strive. In the bowel, millions of differing species of bacteria reside in homeostatic harmony with one other, making our bowels a contented peristaltic paradise. Now if one takes antibiotics for your leg infection for instance, they will pervade the bowel and kill off millions of bacteria.
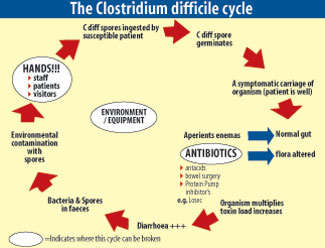
However, some bowel bacteria will be left standing and can use the opportunity to multiply unchecked and dominate the bowel. The one of interest to us is a bacterium named Clostridium difficile – we’ll call it CDIFF for the purposes of this article.
CDIFF is a hardy little bacterium that comes from the Clostridial family. While the Clostridial family may not be instantly recognizable, one will almost certainly be familiar with a couple of nasty diseases that its members cause, namely tetanus and botulism. The bacteria from this family also share the ability to lie dormant in a form known as a spore. A spore is somewhat like a tortoise’s solid shell that protects bacteria from a variety of external stressors – in other words, it gives CDIFF a survival advantage over other bacteria in the bowel. CDIFF also has a couple of toxins. It is these toxins that inflame the large bowel, leading to an illness called colitis.
In its mildest form, CDIFF causes some watery diarrhoea without other problems. But in its most fulminant form, the illness can transform into one of fevers, dehydration, severe abdominal pain and swelling with not only the passage of diarrhoea but also blood and mucus. From this vociferous form, people may need removal of their large bowel or can even die. This life-threatening manifestation of CDIFF wasn't that common; however, about 5-10 years ago, a more virulent clone of CDIFF appeared in the Northern hemisphere where more severe illness was the rule rather than the exception. This clone wreaked havoc across developed countries such as Canada, the United States and the United Kingdom. Death rates from CDIFF infection due to this clone were in the realms of 25 % - an extraordinary figure for an acute infectious disease in the modern medical age.
In summary, so far we know that anyone who takes antibiotics and already has CDIFF in their bowel is at risk of infection. Now, not everyone carries CDIFF in their bowel normally. Carriage of CDIFF in one’s bowels used to be typically associated with hospitalized individuals and older people, especially those in institutions such as nursing homes; however, CDIFF infection is being seen increasingly in younger people from the community with no history of hospitalization.
Another intriguing and worrying discovery in both the developed and developing world is that CDIFF has been identified in raw meats. In other words, it may be picked up through eating. Preceding antibiotic use still remains the most important factor. In fact, so powerful is the effect of antibiotics on wiping out bowel bacteria that people are at risk of CDIFF infection for up to 2 months after completing their course of antibiotics! Any antibiotic can lead to CDIFF infection although penicillins (such as amoxycillin), cephalosporins (such as cephalexin) and clindamycin are the most notorious culprits.
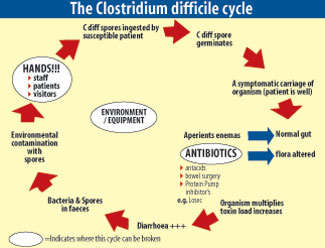 |
Apart from antibiotics, proton pump inhibitors (PPIs) are another group of drugs that are associated with increased risk of CDIFF infection. PPIs are very common and are used to treat peptic ulcers and reflux oesophagitis e.g. omperazole and pantoprazole. The way in which they successfully treat ulcers and reflux is by reducing the amount of stomach acid. Unfortunately, although reducing the acidity of the stomach might relieve these conditions, it also removes an important barrier against infection, not only relevant to CDIFF but also to a number of other bacteria.
At this point, it is worth mentioning that everyone who gets diarrhoea while on antibiotics does not have CDIFF infection. Diarrhoea and other gastrointestinal side effects are common hazards of antibiotics that can occur through a variety of mechanisms. So when should one be suspicious of CDIFF infection? It would be worth considering CDIFF infection if the diarrhoea:
1.Persists during and after a course of antibiotics (up to 2 months after as mentioned above)
2. Is associated with the passage of blood or mucus
3. Is associated with fevers (independent of the infection for which the antibiotics were started), abdominal pain and swelling
If one’s doctor wishes to confirm the diagnosis of CDIFF infection, the simplest and most common test requires a single stool sample which can be tested for the toxins that CDIFF produces. More sophisticated molecular tests and culture tests can be performed but these aren’t as commonly used.
Given the dire illness that CDIFF can precipitate, one wouldn’t be blamed for feeling a sense of hopelessness and concerns that CDIFF infection will inevitably lead one to meet one’s maker in an explosion of bloody diarrhoea and blistering bowels.
Yet although CDIFF infection can be deadly, especially the virulent clone that terrorized the Northern hemisphere, it can be treated. In some cases, even stopping the offending antibiotic is enough to quell the infection. But the mainstay of therapy for this infection caused by antibiotics, is ironically, other antibiotics!
Metronidazole is commonly used for mild cases of CDIFF infection; however, for more severe infections, other agents such as oral vancomycin, must be used. As mentioned earlier, some people are so unwell that their large bowel has to be removed. Given that depleting the bowel’s resident bacteria provides the perfect conditions for CDIFF to multiply and result in infection, the role of probiotics in preventing and fighting CDIFF infection has been examined. Probiotics refer to products that contain bowel bacteria such as Lactobacillus and may be bought in the form of yoghurts, drinks or tablets. The premise is that ingesting these “good bacteria” might restore the microbiological equilibrium of the bowel and “put CDIFF in its place”.
There have been studies looking into this but there are no firm conclusions regarding the role of probiotics in prevention or treatment of CDIFF infection. At the very least, however, they are unlikely to do any harm in otherwise healthy individuals taking antibiotics.
Although well known in Western countries, CDIFF is less of a celebrity in Sri Lanka; however, there is increasing awareness amongst healthcare providers here. In fact, Australia’s foremost authority on the disease (no, not me!), came here earlier this year to talk to Sri Lankan health professionals about this intriguing infection.
CDIFF is almost certainly lurking in the bowels of Sri Lankans from all walks of life. A course of antibiotics may be enough to unleash it upon an unsuspecting victim – so beware and speak to your doctor if you have any concerns.
|