News
TLC until death
‘Where O death is your victory? Where O death is your sting?’ it is queried in the Bible, but as human beings some of us are terrified or fearful of death while others are puzzled as to what lies beyond the grave.
But death is a certainty of life, it is inevitable and for some it seems closer than for others.

Dr. Shama Goonatillake
Not only these men, women and children who seem to be closer to death but also their families are the tender and gentle focus of World Hospice and Palliative Care Day which was marked yesterday with a half-day programme on ‘Caring beyond cure’ organized by the Palliative Care Association of Sri Lanka at the BMICH .
With the powerful theme of this day being ‘Universal Health Coverage (UHC) and Palliative Care – Don’t leave those suffering behind’, Consultant Clinical Oncologist Dr. Shama Goonatillake attached to the Batticaloa Teaching Hospital says the sub-themes centre on the three Cs.
Count – who needs palliative care and who is covered?
Care – which services are covered?
Cost – who will pay for palliative care which is part of UHC and how will they do it?
Death may not have a sting, but in Sri Lanka, the sting is evident with regard to the non-facilities for the provision of palliative care, the Sunday Times learns.
“We are just developing palliative care and are still in the ‘transient period’,” says Dr. Goonatillake, explaining that as a country we began looking at this vital segment only about six years ago. When there is a terminal illness most clinicians assume that “there is no other treatment” after a certain stage, but things have changed over the years globally with modern palliative care and efforts are going in the right direction in Sri Lanka now.
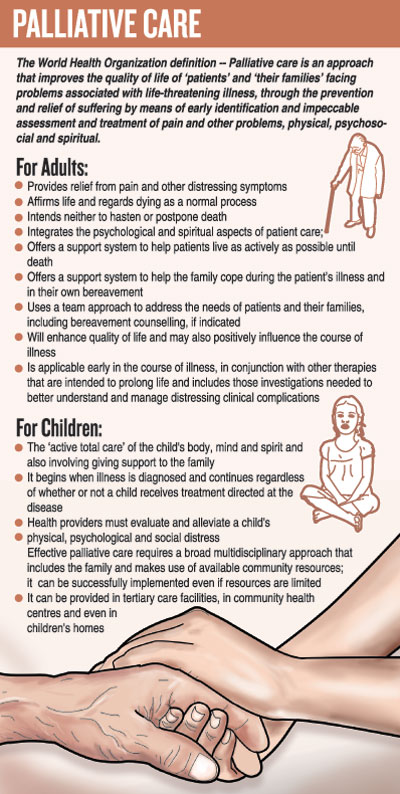
He reiterates that the WHO definition clearly includes not only the quality of life of the patient but also his/her family. (Please see graphic)
Pointing out that initially palliative care was only considered for cancer, Dr. Goonatillake says that now there is whole gamut of diseases which fall under its umbrella. They include end-stage heart, lung (pulmonary), liver and renal (kidney) diseases as well as neurological conditions such as motor neurone disease and dementia; Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome (HIV/AIDS) and also multi-drug resistant tuberculosis (TB).
“It should be the holistic palliative care approach covering the physical, the psychological, the social and the spiritual aspects,” he says, explaining that hospitals most often deal only with the physical aspects. Palliative care must start at the time of diagnosis, but in Sri Lanka it is not happening.
Citing the example of a cancer, which therapy may be able to cure, this Oncologist states that the treatment in the form of chemotherapy or radiotherapy could bring about side-effects. Palliative care will help patients to overcome or alleviate these side-effects. At diagnosis, palliative care may be a very small component, such as if a breast cancer is detected early and surgery, chemotherapy and radiotherapy form a major part of the curative component of treatment. Then palliative care could deal with the side-effects – the pain after surgery, the pain and fatigue after chemotherapy and also psychological and social impacts.
Such palliative care will continue if the person has a relapse or the cancer metastasizes (spreads to other sites). Then the curative component gradually lessens and the palliative component intensifies, he points out.
Dealing with the sensitive end-of-life or terminal stage, Dr. Goonatillake underscores that palliative care does not stop even at the point-of-death. “It should extend not only to the family of the bereaved but also to the carers of the patient who will have emotional trauma.”
The bereaved need “lots of support”, the Sunday Times understands, with the usual mourning period over the loss being about six weeks, which would be natural. But if there is prolonged suffering over the death, then the family will need psychological intervention.
For Dr. Goonatillake, a poignant true-life example comes to mind of a young mother, suffering with metastasized breast cancer, who had a small child. She was his patient. Two years after she died, he had suddenly got a text message from her husband asking him how he was. About a month later he had got another message and then he had realized that it was actually a plea for help from the husband who was still suffering in silence over the loss and channelled him to a Psychiatrist.
Referring to the “normal picture” associated with palliative care, this Oncologist says it is usually linked to providing relief from pain and distressing symptoms.
Although the common symptom is pain, there are about 40 more symptoms which need to be identified and relieved.
“There is a need to understand that in palliative care we respect life, while coming to grips with the fact that dying and death is a normal process. Sometimes healthcare staff thinks that all patients need to be cured. In palliative care, we do not quicken death or slow-down (postpone) death, allowing the patient to suffer.
Euthanasia or mercy-killing is not accepted in palliative care. The aim, however, is to keep the patient as active as possible till death and provide quality of life,” he says, adding that patients with a terminal illness should not be kept as prisoners in their homes but allowed to carry out little tasks – for their satisfaction not to complete the work.
In Sri Lanka palliative care is being administered in an isolated manner, says Dr. Goonatillake, urging that for the implementation of proper palliative care programmes, multi-disciplinary teams should ideally be in place. The team would comprise a Palliative Care Consultant, a Palliative Care Nurse Specialist, a Community Palliative Care Nurse, a Palliative Care Social Service Officer, a Palliative Care Pharmacist, a Physiotherapist, a Counsellor, members of the clergy and volunteers.
| Pain-relief right of every patient and no need to fear morphine | |
| It is the right and not just the privilege of a patient to be pain-free. The disease may not be curable but the pain should and must be controlled, stressed Consultant Anaesthetist Dr. Hemantha Kumarihamy attached to the Neurosurgical Unit of the National Hospital of Sri Lanka, looking at the most basic premise of palliative care. Pointing out that when a person is afflicted by a progressive incurable disease, not only he or she but also the family faces a multitude of problems, Dr. Kumarihamy who is also a Master Trainer in Palliative Care, says that it is essential to give everyone a lot of support.Detailing the strong efforts being made by the Health Ministry along with the Palliative Care Task Force of the Sri Lanka Medical Association, the Palliative Care Association of Sri Lanka, the Consultants at the Apeksha Hospital at Maharagama, to develop a Palliative Care Service, she said that 17 Consultants and 38 nurses, psychologists and social workers across the country are involved as Master Trainers in this common mission. Echoing the need for a holistic approach covering the physical, psychological, social and spiritual aspects when rendering palliative care, Dr. Kumarihamy says as pain is the commonest symptom, its management is crucial, while also taking into account other issues such as immobility, intractable breathlessness, wounds, constipation, nausea and vomiting, to make the patient comfortable. Pain assessment is important, according to Dr. Kumarihamy, and all the different types of pain should be given meticulous attention. The gold standard for pain assessment is self-reporting by the patient as pain is a very subjective feeling and doctors necessarily should build-up a very good rapport with the patient so that he/she is comfortable sharing details about their pain. In the management of severe pain, opioid-like medications such as morphine are “saviours”, she says, urging both doctors and patients not to be fearful of them. “Fear of death, meanwhile, will also cause immense anxiety which entails getting the patient psychological support, while social support will have to come into play when a patient and his/her family face financial issues and the family routine and structure collapse with the challenge of an incurable disease. Spiritual comfort will have to be extended when a patient fears about what lies after death or a very religious patient or his/her family begins to question ‘why me’,” she adds. |
| A ‘good death’ – best place to die is the UK | |
| Taking up the concept of a ‘good death’, Dr. Shama Goonatillake says that the best country to die in would be the United Kingdom (UK) which was ranked Number 1 in 2015 with its Good Death Index being around 93. This is while Sri Lanka was at 65 with an index of 27.“Sadly, there is a higher chance of having a good death in Kenya, Vietnam, Ghana, Mongolia than in Sri Lanka,” he says.Palliative care has been found to yield a positive influence on those suffering from chronic and terminal illnesses. Quoting studies carried out globally, Dr. Goonatillake says that where there was only curative and where there was a ‘mix’ of curative and palliative care, the patients lived longer and had a better quality of life in the ‘mix’ of treatment. He focuses on the situation in Sri Lanka: In 2012-13, there were 13,950 cancer deaths, with 80% dying with moderate to severe pain or in agonyIn 2012-13, there were 100 deaths from HIV, with 50% dying in moderate to severe painWhen the morphine quantities (an indicator of pain control) used medically in the country was calculated, from 2011 to 2013, only 10.1kg had been used per year on average. How many pain-free deaths can be managed with this amount of morphine, he asks, doing a quick calculation – it would only be 24% of these deaths that can be managed and that too meeting only the minimum demand from deaths due to cancer and HIV, excluding all other illnesses. The country would otherwise have needed a minimum amount of 69kg of morphine to cover this group alone. While some clinicians argue that morphine is not available, others are reluctant to prescribe this pain-controlling medication due to several myths associated with morphine, according to him. The myths are: Myth — Morphine causes multi-organ failureMyth – Morphine sets off respiratory failure. This can occur only if there is an overloading of morphine, while this medication is, in fact, good for shortness of breath in lung metastasis. |

