News
Baby delivered and tumour removed in single operation
View(s):It is a moment of tenderness between mother and baby. S.D. Kanchana Lakmali, 34, holds her baby-daughter close, just a week-old and yet to be named, and looks into her bright little eyes.

Kanchana and her newborn. Pix by Amila Gamage
Unexpected was this pregnancy, so many long years after the birth of her older son and daughter who are 19 and 16 years old.
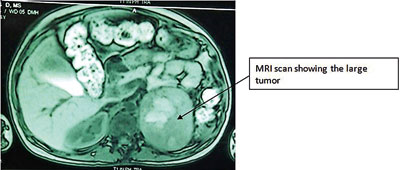
But Kanchana is thankful, for she believes that it is this newborn who helped save her life. It was a double-delivery for Kanchana on October 11 – her baby-daughter weighing 2.3kg and a huge, rare and dangerous tumour of the adrenal gland tissue taken through a single surgical incision on her abdomen.
“Mage bade loku gediyak thibila thiyenawa,” Kanchana who is from Pannala tells the Sunday Times when we meet her and the baby on Tuesday just after noon in Ward 5 of the De Soysa Hospital for Women down Kynsey Road, Colombo. The tumour was a pheochromocytoma, the size of a small coconut.
Kanchana is alive to tell her tale of survival because many medical specialties both at the National Hospital of Sri Lanka (NHSL) and the De Soysa Hospital, duly assisted by nursing staff, worked in tandem. Those at the Kurunegala Hospital had also taken all the necessary measures to ensure her safe arrival in Colombo.
This is testimony to how Sri Lanka’s State health sector works to give of its best to humble patients such as Kanchana. It is also proof of the success of the essential multidisciplinary approach in saving lives.
Those who were involved in this complex procedure were the NHSL Endocrine Team comprising Dr. Noel Somasundaram, Dr. Manilka Sumanatilleke, Dr. Chaminda Garusinghe, Dr. Achini Wijesinghe and Dr. Madushani Karunanayake, while the De Soysa Hospital’s Obstetric Team consisted of Dr. M.A.K. Perera, Dr. S.N. Samarakkody, Dr. P.L.A. Sirisena and Dr. H.N.D. Silva. The Anaesthetic Team was headed by Dr. Marie Fernando and the Surgical Team led by Dr. B.G.N. Ratnasena included Dr. M. Mathurageethan and Dr. T.A.D.S. Perera.
Explaining that she did not know that she was carrying a large tumour, Kanchana recalls how from about five years ago she experienced a “gasma” in her chest, breathlessness, dizziness and feeling faintish. She would throw up too.
She would take a little medication from private doctors and continue with her work. In fact, she had worked in West Asia for 13 years, first in Qatar and then in Jordan, returning home only two years ago. She would have 10-minute bouts of hathiya (panting), stop work and then resume her chores after they passed.
Back in Sri Lanka, life got into a routine and even though she was taking precautions, sometimes not too rigidly, Kanchana found that she was expecting another baby. Thirty-four weeks (over eight months) into her pregnancy, on an early morn, she became very ill, with non-stop vomiting and very laboured breathing. Rushed by her husband, Liyanage Roshan, to a private doctor whose clinic was open 24-hours, an electrocardiogram (ECG) was done and the couple advised to go to the nearest hospital immediately.
Dambadeniya Hospital was the closest and when they arrived there, Kanchana was transferred to the Kurunegala Hospital where it was straight to the Intensive Care Unit (ICU) that she was taken.
“I couldn’t breathe and my hands and feet were shivering violently,” says Kanchana, adding that a battery of tests including echocardiograms and scans were done there, after which she was once again transferred to the De Soysa Hospital on the night of October 7. “Wakugadu uda bayanaka gediyak thibba,” she explains.
Pointing out that it was not until she was in late pregnancy that the life-threatening tumour in her adrenal gland was detected, a medical team member says that even in non-pregnant patients the removal of such a tumor is dangerous and is done only in specialised centres, after a great degree of precautions are taken and preparations made.
As soon as Kanchana was transferred from the Kurunegala Hospital to the De Soysa Hospital, doctors here were awaiting her arrival for immediate assessment and stabilisation with medications to block the production of excessive hormones, the Sunday Times understands.
A pheochromocytoma is a rare neuroendocrine tumour of the medulla of adrenal glands. While the adrenal glands are located above the kidneys, they produce a number of hormones which control the heart rate, metabolism and blood pressure. The pheochromocytoma derives its name from the Greek phaios ‘dark’, chroma ‘colour’, kytos ‘cell’, -oma ‘tumour’.
The usual symptoms of such a tumour are abdominal pain, chest pain, irritability, nervousness, pallor, palpitations, rapid heart rate, severe headache, sweating and weight loss with other signs being hand tremors, high blood pressure and sleeping difficulty.
It had been found that Kanchana was suffering from a hereditary condition known as neurofibromatosis that causes tumours in the nerves and adrenal glands.
The multi-specialist team had then decided that it was best to deliver the baby and the tumour in a single surgery or a combined operation, working throughout the weekend to get Kanchana ready.
“A pheochromocytoma produces adrenaline and the heart rate and blood pressure can shoot to dangerous levels when it is handled during surgery. This, in turn, creates a volatile and highly unstable situation,” the medical team member said, adding that the patient can die of the uncontrolled beating of the heart or a rise in blood pressure.
The opposite, meanwhile, can happen after the operation, as the blood pressure can plummet to extremely low levels when the constricted arteries relax too much after the removal of the tumour. The other issue faced by the doctors was that the baby was filling almost the entire abdominal cavity and pressing on the tumour.
“On October 11, after extensive medications and preparations that would block the adrenaline from the adrenal tumour, we set about extracting both the baby and the growth through one cut,” the medical team member pointed out, explaining that first the baby was removed by Consultant Obstetrician and Gynaecologist Dr. Perera and his team.
Subjected to a barrage of hormones by the tumour while in the womb, the baby was not breathing well and in stepped Consultant Paediatrician Dr. Nalin Gamaethige and his Neonatology Team to resuscitate and ventilate her, the Sunday Times learns.
Like clockwork, when next moved in Consultant Surgeon Dr. Ratnasena and his team to remove the large tumour, Kanchana’s blood pressure had shot up to more than 260mmHg (the normal is 120mmHg) with Consultant Anaesthetist Dr. Fernando and her team having the unenviable task of controlling the blood pressure with a cocktail of rapid-acting drugs.
“Once the tumour was out it was much easier to manage the situation. But as there could be no complacency, mother and baby were managed in the De Soysa Hospital’s ICU,” the medical team member added.
And on Tuesday when the Sunday Times meets Kanchana and her pretty baby, they are out of the ICU, having come to Ward 5 the day before.
“Gediyai, babai dekama eliyata gaththa,” smiles Kanchana, adding that her husband has sought out the letters from which the little one’s name should be made.
Kanchana is eagerly awaiting the return home, for the newest addition to the family has only been seen by her husband. Introductions are pending to the baby-girl’s big aiya and akka.
As the baby gives a wide yawn, a sharp look around and a tiny cry, signalling that she wants her Amma’s sole attention, we bid adieu to Kanchana sans her tumour but with her newborn in her arms.

