Fighting filaria: The battle is almost won
The good news is that Sri Lanka is winning its war against Lymphatic Filariasis, the bad news is that undetected, high density pockets of infection may remain, especially in the North and East, areas that present the Anti-Filaria Campaign with a new challenge. “We are at the elimination stages now according to the WHO guidelines which is below 1%, our rate is 0.03%,” said Dr. Udaya Ranasinghe, Director of the Anti-Filariasis Campaign, Ministry of Health in Colombo.
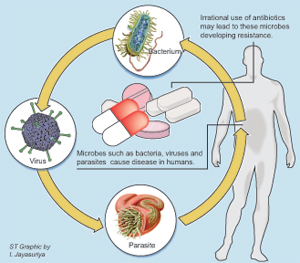
Lymphatic Filariasis is an infection caused by filarial worms, namely Wuchereria bancrofti, Brugia malayi or B. timori. Hitching a ride onto humans through the bite of an infected mosquito, the worms settle in lymphatic vessels – the network of vessels that drain fluid from the tissues and carry infection-fighting cells. Here they develop into adults and produce microfilariae (Mf). When a mosquito bites an infected person, the insects pick up these Mf. Inside the mosquito, the tiny worms begin to develop, until over the next seven to 21 days they have reached a larval stage and can then move from the mosquito to the next human it bites. Filariasis is associated with genital disfigurement, kidney damage and lymphoedema or swelling of the limbs, which give the infection its other name – Elephantiasis.
At the Anti-Filariasis Campaign centre in Colombo, Dr. Chamila Nagodabithana helps patients manage the symptoms of their infection. While swelling of the lower limbs is most often seen in Elephantiasis, Dr. Nagodabithana says that in women, swelling of the breasts is common and in men, it is the scrotum. Initially, the swelling seems soft and very mild but can easily worsen over time. The skin in the area can appear reddened and itch before swelling appears. “With the swelling there is always a tendency for the other germs that are already living on the skin to get through even a small wound that will give rise to cellulitis which will aggravate the condition more,” he explains, attributing the dark, thickened skin so commonly associated with the Elephantiasis to “the continuous, repeated infections of the Edema site.” Fungal infections are also common.
As with so many other conditions, early diagnosis and careful, consistent management can make a big difference to patient’s life. In cases where the adult worm is still in the body, drugs can be prescribed to kill it – which was what was done during the rounds of Mass Drug Administration carried out according to WHO guidelines. However, most of the patients who make their way to the clinic no longer have a live worm in them. “The life span of the worm is about five to seven years and whether you take treatment or not, that worm will die,” says Dr. Nagodabithana. However, Mf in the body can indicate that it was once there and the worm’s demise does not undo the damage already done to the lymphatic system.
“There is no role in giving DEC (drug) at that point so what we manage is the disability part of the problem and the edema,” says Dr. Nagodabithana. Part of the process is washing the limb very carefully. He recommends using normal, clean water and mild baby soap. The limb should then be soaked in a little bit of condis diluted in lukewarm water (the water must be pink not darker) for 8 – 10 minutes, then removed and allowed to air-dry. Where needed, a doctor will also treat wounds and infections with anti-microbials and anti-fungals since subsequent skin infections are to be considered in long term management of the condition.
For the patient at home Dr. Nagodabithana recommends that whenever possible he or she should do exercises which will encourage the fluid accumulating in the limb to drain away. “When the patient is sleeping, we advise them to lift the foot end of the bed, so that will also help.” Bandaging the affected limb must be done correctly, from bottom to top, and is best done in the morning when the edema is typically at its least intense. We have seen patients who have come at the early stages and have actually adhered to the protocols we recommend who have done very well, he says, explaining that with no skin changes the limb looks very normal. Equally, neglecting it can aggravate the problem.
For the Anti-Filaria Campaign dealing with affected cases at their clinics is one of their primary focuses right now. The other is ensuring that the infection doesn’t get a foothold in the country again. This is an old battle for the island, which became in 1947, the first country in the world to launch its own national Anti-Filariasis Campaign. In 2002, the authorities initiated a WHO-recommended MDA programme in eight endemic districts including Galle and Puttalam. The programme ran for five years. It’s difficult to confirm the number of patients because at the very beginning the infection can be asymptomatic, reveals Dr. Sunil Settinayake, one time director and now a Special Coordinator at the campaign.
Many people pick up the infestation during childhood, and it can take years for the symptoms to appear. Some patients however will show signs such a chronic cough and fever, said Dr. Settinayake.
To monitor the transmission of the disease, the campaign is even now testing sample populations of school children in what used to be high-incidence areas. These children, born after 2007, were never included in the MDAs that were administered between 2001 – 2006, so if Mf appear in their blood it is evidence that fresh transmissions are occurring. The process can be a challenging one, as current tests require blood samples to be taken and often at night when the Mf in the blood are most easily detectable. They are also manually collecting mosquitos to check for the infection. Researchers working in the field are looking at developing tests that require urine samples instead and will be easier to take into the field, requiring less in terms of expensive equipment and skilled personnel.
Luckily, treatment is quite affordable. The campaign has begun to open new Filaria testing centres (the most recent is one in front of the Provincial Director’s office in Kurunegala) and hopes to make sure that every teaching hospital and base hospital has their own easily accessible testing centre for patients. Having beatback the infection, vigilance is now required to make sure it doesn’t return.
For more information, contact the Anti-Filaria Campaign on 0112506249 or visit them at 555/5, Public Health Complex, Elvitigala Mw., Colombo 5.
Follow @timesonlinelk
comments powered by Disqus