News
No monkeypox in SL
 Monkeypox is riveting the attention of the world.
Monkeypox is riveting the attention of the world.
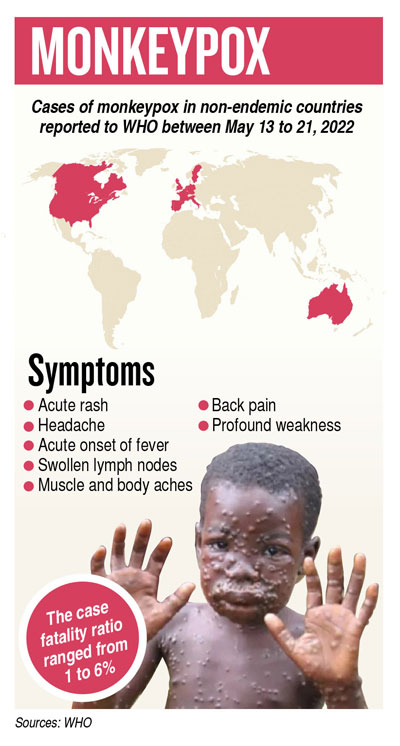
Usually endemic to Central and West Africa, currently cases of this not-deadly viral disease have been detected in non-endemic United States of America, several European countries including the United Kingdom, Israel and Australia.
“No cases have been detected in Sri Lanka or this region,” said Dr. Jude Jayamaha, referring to a recent spike as over 100 cases were confirmed or suspected in Europe.
He says that the risk of monkeypox spreading in Sri Lanka is minimal. The Quarantine Unit of the Health Ministry is vigilant against the dangers of imported cases. The Medical Research Institute’s Department of Virology has the experts who are working with the support of the Regional Office of the World Health Organization (WHO) to establish a novel multiplex PCR to detect monkeypox.
Quoting the WHO, he says that the name ‘monkeypox’ came about as the disease was first identified in colonies of monkeys kept for research in 1958. It had been detected in humans in 1970.
What is monkeypox and is it deadly?
Monkeypox is an uncommon, self-limiting viral disease. It is usually not deadly. Severe cases occur more commonly among children.
The severity of monkeypox is related to the extent of virus exposure, the person’s health status and nature of complications. Underlying immune deficiencies may lead to worse outcomes. The extent to which asymptomatic infection may occur is unknown.
The case fatality (death) ratio of monkeypox has historically ranged from 1 to 6% in the general population and has been higher (around 3 to 6%) among young children.
The complications of monkeypox can include secondary infections, broncho-pneumonia, sepsis, encephalitis and infection of the cornea, with ensuing loss of vision.
How does it spread?
Transmission usually occurs through close contact with infected animals such as rodents and monkeys and is limited between people. Animal-to-human (zoonotic) transmission can occur from direct contact with the blood, bodily fluids, skin or mucosal lesions of infected animals. In Africa, evidence of monkeypox virus infection has been found in many animals including rope squirrels, tree squirrels, Gambian pouched rats, dormice and different species of monkeys.
The natural reservoir of monkeypox has not yet been identified, though rodents are believed to be the most likely reservoir.
Eating inadequately cooked meat and other animal products of infected animals is a possible risk factor.
Human-to-human transmission can result from close contact with respiratory secretions, skin lesions of an infected person or recently-contaminated objects. Transmission via droplet respiratory particles usually requires prolonged face-to-face contact, which puts health workers, household members and other close contacts of active cases at greater risk. However, the longest documented ‘chain of transmission’ in a community has risen in recent years from six to nine successive person-to-person infections.
What are the symptoms?
The symptoms are fever, muscle aches and swollen lymph nodes. A chickenpox-like rash (fluid-filled blisters) are also found on the face, hands and feet and sometimes on the mouth, genitals and eyes. The symptoms usually last from 2 to 4 weeks.
What is the treatment?
Treatment is mainly supportive. While symptoms such as fever are managed, patients are given fluids and food to maintain their nutritional status. Tecovirimat, an anti-viral drug developed to treat smallpox, has been licensed for monkeypox in January 2022 based on data in animal and human studies. It is, however, not widely available worldwide yet.
If there is a secondary bacterial infection, that would be dealt with through antibiotics.
Is there a vaccine?
Several vaccines developed to prevent smallpox provide 85% protection against monkeypox, while a newer anti-smallpox vaccine (MVA-BN also known as Imvamune, Imvanex or Jynneos) was approved in 2019 to prevent monkeypox. But it is not widely available.
According to the WHO people who have been vaccinated against smallpox in the past will also have some protection against monkeypox. The original smallpox vaccines are no longer available and people below the age of 40-50 years are unlikely to have been vaccinated, since vaccination against smallpox ended in 1980 after it became the first disease to be eradicated. Some laboratory personnel or health workers may have been vaccinated with a more recent smallpox vaccine.
The best way to say that you found the home of your dreams is by finding it on Hitad.lk. We have listings for apartments for sale or rent in Sri Lanka, no matter what locale you're looking for! Whether you live in Colombo, Galle, Kandy, Matara, Jaffna and more - we've got them all!

