| HELPING
TO LIVE WITH PARKINSON’S
By Smriti Daniel
Parkinson's
disease does not have a cure. In the past, for those
who contracted it, the years ahead seemed to hold only
steady decline. More recently, however, a proactive,
life-affirming approach has been adopted at the National
Hospital's Movement Disorders Clinic. A team consisting
of neurologists, neurosurgeons and therapists are battling
the disease using cutting edge technology and simple
techniques -so that victims of the condition may live
a near normal life.
Parkinson's disease is one of the most common manifestations
of a movement disorder, says Dr. Ranjini Gamage, Consultant
Neurologist at the National Hospital. "A good 90
to 95% of the (movement disorder) patients belong to
Parkinson's disease," she adds.
 |
| Electrodes inserted into the patient's
brain allow the surgeon to monitor the brain and
to locate the subthalamic nucleus |
Dr.
Gamage who sees her patients on Mondays at the Movement
Disorders Clinic explains that it is the only one of
its kind in Sri Lanka. Having opened two years ago the
clinic treats about 1000 patients with Parkinson 's
disease.
 |
| A monitor showing the pattern
of electrical impulses in the brain as recorded
by the electrodes. |
Many
who come there are unaware they have the disease. Dismissing
it as the natural effect of aging, some leave it until
the illness is in its last stages. At the onset of the
disease, a patient will probably complain of tremors,
rigidity and slowness in movement, (known as hypokinesia)
warns Dr. Gamage. "When you have all three, then
patients have difficulties in their day-to-day activities,
like standing straight, turning, feeding or writing,"
she says. Poor balance and postural instability are
common as is the difficulty in walking leading to a
pattern of walking - known as the Parkinsonian gait.
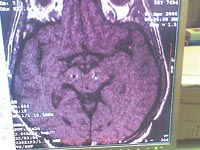 |
| Post-operative scan showing the
correct placement of electrodes on both sides of
the brain. |
While
it is most common amongst the elderly, the occasional
young person has been known to fall victim to the disease.
Genetic disorders, certain medications (such as those
prescribed for schizophrenia), vascular disorders and
other environmental factors have been known to trigger
Parkinson's like symptoms. The actual disease is marked
by the progressive deterioration of the nerve cells
in the part of the brain known as the substantia nigra.
Dopamine, which is one of the substances used by cells
to transmit impulses, is normally produced in this area.
Naturally, the deterioration in the substantia nigra
reduces the amount of dopamine being produced, which
in turn leads to an imbalance between dopamine and other
neurotransmitters such as acetylcholine. "As a
net result of the chemical imbalance that occurs between
the two neurotransmitters certain areas of the brain
become hypo-active while others become hyper-active,"
reveals Dr. Gamage.
"Therefore the treatment of Parkinson's is directed
towards increasing the dopamine levels in the brain
or decreasing the acetylecholine levels," says
Dr. Gamage adding that "this is done by giving
various drugs." The aim is to balance the chemicals
in the system, and the mainstay of treatment remains
medical. "The clinic also screens Parkinson's patients
for advanced management," says Dr. Gamage, explaining
that this might involve the use of new drugs or advanced
surgical techniques.
It must be understood that there is currently no cure
for Parkinson's. The disease is both chronic and progressive,
meaning that symptoms will continue and worsen over
time. All treatment is geared simply towards retaining
normal function for as long as possible.
Surgery,
in particular, is a possibility when the medication
has ceased to have any effect. Dr. Gamage explains that
this occurs over time as patients develop a tolerance
- requiring more and more medication to control their
symptoms. This stage is reached in 5 to 10 years time.
"We do this (surgery) for patients who don't have
any other hope," says Dr. Gamage, "because
at this point the drugs have failed."
Dr. Sunil Perera, a neurosurgeon at the National Hospital
says that there are essentially two options when it
comes to surgery -Pallidotomy and Deep Brain Stimulation
or DBS. Pallidotomy has been around for some time now,
says Dr. Perera, explaining that the operation involves
the precise destruction of a small area (the globus
pallidus) in the deep part of the brain that causes
symptoms. He warns that this is a one-time only procedure,
as it destroys brain tissue irrevocably. Also, it can
only be done on one side of the brain. In the end, it
only offers relief from symptoms for 2 to 3 years, after
which problems will return. Not surprisingly, Dr. Perera
thinks that Pallidotomies will soon be a thing of the
past.
Deep Brain Stimulation on the other hand is effective
for far longer - even up to 12 years. Dr. Perera who
was the first and only surgeon in the country to do
so, conducted a DBS operation last year. Since then
five such procedures have been undertaken with successful
results. "This operation is unique to the country,"
he says, explaining that he travelled to several other
countries to learn how it was done.
Experienced neurosurgeons from India were also brought
down to work with the team in the initial stages. The
operation is complicated and is moreover a team effort.
"The neurosurgeon must work with a neurologist
for it to be successful," says Dr. Perera, explaining
that the patient remains conscious throughout the surgery,
enabling the neurologist to determine whether there
is a significant improvement or not.
The results are almost magical and can be seen at once,
he says. In DBS, electrodes are placed in a small part
of the brain called the subthalamic nucleus or globus
pallidus. The electrodes are then connected by wires
to a type of pacemaker device, called an impulse generator
or IPG, which is implanted under the skin on the chest,
below the collarbone. Once activated, the device sends
continuous electrical pulses to the targets, blocking
the impulses that cause tremors. It does not destroy
brain tissue and has fewer risks than older, more destructive
surgical methods, he explains.
However, it is expensive. The electrodes themselves
can cost over a million rupees, which is to be expected
as it is the most advanced surgery for Parkinson's in
the world, says Dr. Gamage. The National Hospital is
not equipped to handle a DBS operation, so they have
been conducted in private hospitals such as the New
Asiri Surgical Hospital.
In the meantime, the Movement Disorders Clinic continues
to dispense medicine and advice every Monday to patients
who come from all over the island. Part of the programme
is several therapy sessions which are geared to help
Parkinson's patients control their symptoms and make
daily life easier.
Parkinson's patients are commonly affected with speech
related difficulties, says speech and language therapist
Saumya Ratnayake. Difficulty in producing sounds results
in speech changes; words become slurred and the tone
becomes monotonous. A loss of facial expression is characteristic
of sufferers of Parkinson's disease and is known as
"masking”. "They also have difficulty
in swallowing," says Ms. Ratnayake, adding that
memory problems compound the situation as patients are
often literally at a loss for words.
To cope with this, she recommends patients do simple
things, such as take deep breaths or change posture
to make it easier to speak louder. Similar methods are
employed by Sampath Abeyawardana who works as a physiotherapist
at the clinic. He reveals that standing up, walking
and even turning can become ordeals for Parkinson's
patients. For instance, a patient might get frozen in
one place and find himself unable to take a simple step
forward. The solution is to take an extra large step,
almost as if one were stepping over an obstacle. Other
simple exercises increase muscle strength and flexibility
and correspondingly decrease the chance of nasty falls.
Such techniques are designed to keep the patient mobile
and independent for as long as possible, reveals occupational
therapist Nandana Welage. During the half - hour sessions
that the team conducts, patients and caregivers learn
more about coping with the practical day to day aspects
of the disease. It is easy for them to become depressed,
says Mr. Welage, considering that the degenerative aspect
of the disease seems to leave little room for hope.
However, moulding the environment to suit the patient
helps considerably. Modifications to toilets, utensils
and even pens can keep a patient self-reliant for much
longer periods of time. For instance, cups can be made
heavier and with larger handles, enabling someone with
severe tremors to pick it up with ease. Such options
provide a stronger sense of control when living with
Parkinson's disease.
In the end, it is the emotions that need the most strengthening.
Both patients and their families can end up battered
by this ravaging disease. Depression, fear and anxiety,
compounded by memory difficulties and in extreme cases
dementia make for tough going….and it is perhaps
in this part of the struggle that the Movement Disorders
Clinic and its staff will make their presence most felt.
| 