More than a fighting chance for little hearts
All set. Very soon Sri Lanka’s first-ever Human Heart Valve and Tissue Bank at the Lady Ridgeway Hospital (LRH) for Children in Colombo will be fully functional.

Dr. Duminda Samarasinghe
“We already have about 12 human valves in storage and in a month or two will be able to graft them in very ill children with congenital (present at birth) heart disease,” says Paediatric Cardiologist Dr. Duminda Samarasinghe whose dream this has been for a very long time.
These valves will help save many lives, MediScene learns, and the LRH team, which includes Paediatric Cardiologists and Paediatric Cardiac Surgeons, is hoping to undertake at least three or four surgeries a month.
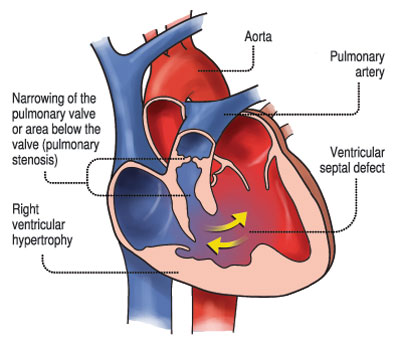
Dr. Samarasinghe explains that they would initially start with children suffering from Tetralogy of Fallot. In a majority of these patients, the pulmonary artery is not formed. (See box)
Commonly known as blue babies, these children suffer from cyanotic heart disease, which results in a low blood oxygen level. They form about 7-10% of those affected by congenital heart disease, it is learnt.
The calculation is simple but for the families who have children with congenital heart disease it is heart-breaking. With around 2,000 children being born with congenital heart disease (caused by a problem with the structure of the heart) every year in Sri Lanka, around 200 would be hit by cyanotic heart disease.
Congenital heart disease may involve the walls of the heart, the valves of the heart and the arteries and veins near the heart and disrupts the normal flow of blood through the heart, MediScene understands.

Jill Davies
Taking MediScene through the processes, Dr. Samarasinghe says that after obtaining consent ethically, from the closest family member, the team would harvest the heart of a dead person, within a few hours of death in a clean environment within the mortuary. The cadaveric donor should ideally be a child or young adult who has not had calcification (build-up of calcium) of the blood vessels or atherosclerosis (plaque build-up in the arteries).
The heart would be placed on the Static Transfer Box with double locks, from the side of the ‘least’ sterile room and passed into the ‘highly’ sterile inner room with filtered air in the Human Heart Valve and Tissue Bank. Here the heart will be dissected in a special Bio-safety Cabinet, harvesting the aortic valve, the aorta, the pulmonary artery and the pulmonary valve. These valves and vessels will also be measured with an accurate record being kept.
The harvested valves and vessels will then be kept in an incubator and treated with antibiotics to ensure that there are no bacterial or fungal growths and stored. The storage is in nitrogen vapour at a temperature of -150°C under gradual gradient freezing, says Dr. Samarasinghe, explaining that they can then be kept for as long as five years.
When the Paediatric Cardiac Surgeons require a vessel or valve for grafting, those in storage would be released, depending on the size requested and there would be a gradual warming up of the vessel or valve to body temperature.
Currently, the children who need replacement of their pulmonary arteries get bovine (cattle) or porcine (swine) artificial vessels imported at high cost from the United States of America.
Earlier, Consultant Paediatric Cardiothoracic Surgeon Dr. Kanchana Singappuli explained the “challenges” when using these conduits prepared from the jugular veins of these animals. There would be a shortage of the two extremes — big and small vessels.
 The vessels from human cadavers are longer lasting substitutes as against the others which are shorter lasting. The artificial vessels do not last as children have high calcium metabolic rates which, in turn, lead to calcium deposits forming (calcification) on these arteries, it is learnt.
The vessels from human cadavers are longer lasting substitutes as against the others which are shorter lasting. The artificial vessels do not last as children have high calcium metabolic rates which, in turn, lead to calcium deposits forming (calcification) on these arteries, it is learnt.
The state-of-the-art Human Heart Valve and Tissue Bank has been set up with the support of 18 Rotary Districts across the world which extended a helping hand to the Rotary Foundation to raise US$ 400,000 (around Rs. 60 million), with the Rotary Club of Colombo Fort acting as facilitator. While Rtn Sushena Ranatunga was instrumental for the project, those actively involved included then Rotary District Governor Gowri Rajan.
The funds for the construction of the building amounting to Rs. 20m were from the Health Ministry.
Once fully-functional, the bank would also benefit adults diagnosed with congenital heart disease. It can also be expanded to store other tissue including skin for burn victims and preserve ovarian and testicular tissue of those who have to undergo chemotherapy and radiation.
| Pulmonary atresia Pulmonary atresia is a form of heart disease in which the pulmonary valve does not form properly. The pulmonary valve is an opening on the right side of the heart that regulates blood flow from the right ventricle (right side pumping chamber) to the lungs. This affects the oxygenation of the baby’s blood. | |
| Team effort  A hands-on training session in progress The all-important team which is making the Human Heart Valve and Tissue Bank a reality include the Consultant Paediatric Cardiologists, the Consultant Paediatric Cardiac Surgeons, four graduate nurses, Advisor Dr. Renuka Sornarajah and the Manager of the Oxford Cell and Tissue Biobank, United Kingdom (UK), Jill Davies who has provided invaluable advice. “We used the same prototype used in Oxford, encompassing the right training and harvesting the right quality tissue for transplantation,” said Ms. Davies, adding that as such the standards are similar to those in the UK. In December last year, Ms. Davies provided hands-on practical training to the staff here, working with pigs’ hearts. “Valves will save the lives of children in Sri Lanka – that’s why we are here to share our knowledge,” she says. Meanwhile, Dr. Sornarajah’s role is to provide guidance on international quality and safety standards. With a doctorate from the University of Cambridge, she has worked as a scientist in the UK, Singapore and Australia and has much technical expertise in setting up new laboratory facilities and processing many types of tissues and cells used for transplantation. She is working on an honorary basis. |

Doing it the right way


