News
Standard stroke care needs unmet yet
The message was loud and clear, not being shouted from the rooftops but from the 8th floor of a building of the National Hospital of Sri Lanka (NHSL).

Consultant Neurologist Dr. Padma Gunaratne making a strong plea on behalf of the ‘voiceless’ stroke patients. Pix by M.D. Nissanka
Giving voice to the voiceless stroke victims was Senior Consultant Neurologist Dr. Padma Gunaratne who is also NHSL’s Head of the Institute of Neurology.
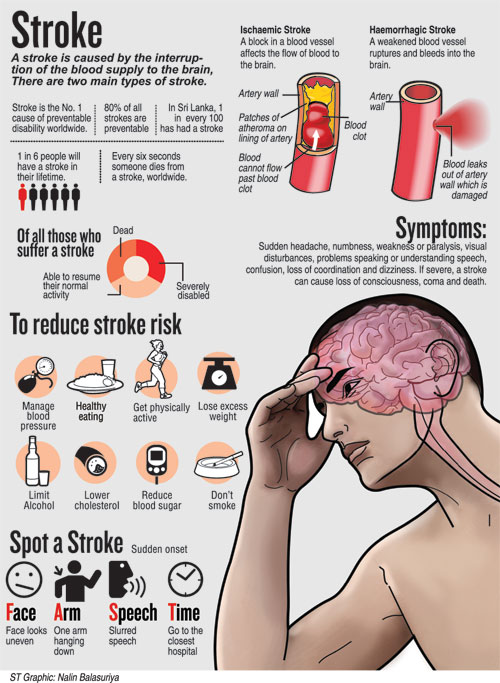
For, stroke is a killer as well as a major harbinger of disability – it is the leading cause of death and disability second only to heart (cardiovascular) disease. Stroke is also the 3rd leading cause of hospital deaths, on par with cancer.
Dr. Gunaratne was urging and pleading for more facilities including multidisciplinary care for those afflicted by stroke, on the afternoon of August 15 at the NHSL’s National Epilepsy Centre auditorium in the presence of a distinguished gathering including Health Minister Dr. Rajitha Senaratne.
Creating a powerful image of the devastation of ‘brain attacks’, she had in hand, facts and data, for along with several hospitals and very supportive Consultant Neurologists, everything is now online.
The occasion was the launching of the much-needed Sri Lanka Stroke Clinical Registry (SLSCR).
It was the analysis of data from five hospitals, the NHSL and the Colombo South, Kandy, Jaffna and Karapitiya Teaching Hospitals, for the six-month period from November 1, 2016 to April 30, 2017 that was presented covering 2,735 stroke patients. (See box)
The data collection had begun at the NHSL initially, with other hospitals joining in.
“This has helped us to highlight the fact that we are falling short of the ideal standard of care for stroke patients,” Dr. Gunaratne pointed out, stressing that there is room for improvement. “Much has been done, but much more needs to be done.”
Detailing Sri Lanka’s progress in stroke care, she said that the country introduced clot-busting medication (thrombolization) at the NHSL in 2008 and several more major hospitals later, for patients who had suffered ischaemic strokes if they arrived at the hospital within 4.5 hours of onset. Each dose of rtPA (re-combinant tissue Plasminogen Activator) costing Rs. 100,000 has been provided by the government without interruption, helping many patients.

Consultant Neurologist Dr. Senaka Bandusena detailing the data collected by the Sri Lanka Stroke Clinical Registry
What is also crucial in stroke treatment and management, according to this Neurologist, is multidisciplinary care in dedicated Stroke Units with doctors, nurses, physiotherapists, occupational therapists, speech therapists, counsellors and social workers in attendance.
Can we be happy with what we have, asked Dr. Gunaratne. “We have a long way to go and in general, stroke patients do not have adequate facilities, as currently what is needed are dedicated beds allocated for them in Stroke Units.”
Her lament was that it is not a problem of budgets or allocations, but a seeming sluggishness in the delivery of service. “It’s occurring at snail’s pace.”
The SLSCR, a web-based platform, is a joint initiative of the Health Ministry, the World Federation of Neurology and the World Stroke Organization and will not only help to share but also disseminate crucial information on stroke within Sri Lanka. It has collected and will continue to document information on hospitalized stroke patients to enable better decision-making at all levels of care, the Sunday Times learns.

NCD Directorate Head Dr. Champika Wickramasinghe addressing the gathering
While the project was implemented under an Advisory Committee chaired by Health Ministry Director-General Dr. Jayasundara Bandara and the close watch of Dr. Gunaratne and Consultant Neurologist Dr. Senaka Bandusena attached to the Colombo South Teaching Hospital, the nitty-gritty was deftly handled by Dr. Vijayabala Jeevagan.
It was under the ministry’s Second Health Sector Development Project that the Directorate of Non-Communicable Diseases (NCDs) headed by Dr. Champika Wickramasinghe provided funding for it.
Walking the audience through the SLSCR, it is Dr. Bandusena who explains that the data collection was carried out at the point of care – registration of patients, admission and discharge, with a three-month follow-up through a telephone call — by research assistants using Tablet PCs.
The second phase will see nurses being mobilized as research assistants to maintain the registry. The need of the hour is to ensure that the SLSCR continues feeding vital data on strokes in Sri Lanka to enable stroke treatment and management to be taken to a higher level.
| Thrombectomies to be launched at NHSL | |
| Thrombectomies (removal of clots from blood vessels) for large anterior occlusions (blocks) in the brain will be launched at the NHSL in a few months, announced Dr. Padma Gunaratne, appreciating the support provided by the Health Ministry and NHSL Director Dr. Anil Jasinghe for the arrangements being put in place and the provision of devices. |
| SLSCR an eye-opener regarding stroke-care | |
The findings of the Sri Lanka Stroke Clinical Registry (SLSCR) which looked at 2,735 stroke-patient admissions to the NHSL and the Colombo South (Kalubowila), Kandy, Jaffna and Karapitiya Teaching Hospitals are an eye-opener, showing clearly the direction in which Sri Lanka should head with regard to stroke-care.The male:female ratio of the patients was 57%:43%  A long and hard look at the data collected by the Sri Lanka Stroke Clinical Registry, by (from the right) Health Minister Dr. Rajitha Senaratne, NHSL Director Dr. Anil Jasinghe and Health Services Director-General Dr. Jayasundara Bandara Of the total number, 72% suffered ischaemic strokes; 19% intra-cerebral haemorrhagic strokes; and 9% transient ischaemic attacks (TIAs) |

