News
A first at Kalubowila Hospital
Married for 10 long years, with her biological clock ticking, she and her husband longed to have a baby.
It was to the pioneering Professorial Obstetrics and Gynaecology Unit of the Colombo South (Kalubowila) Teaching Hospital that they came, seeking help.

The pioneering team (from left) are Dr. Madura Jayawardane, Dr. Dhammike Silva, Dr. Seetha Alwis, Dr. Chinthana Hapuachchi, Dr. Dinesh Biyagama, Dr. M. Kopalakrishnan and nurses K.C.M.N. Kulasekara, H. Malawiarachchi and E. Ruwani Sandamali
The ‘time’ was right. For, although unfortunately there would be no baby for 41-year-old Kumari* from Horana, fortunately her life would be saved.
Five small incisions on her tummy would allow a minimally-invasive laparoscopic or keyhole procedure to be performed on her.
It is probably the first laparoscopic procedure to be performed in the para-aortic region of the body by gynaecologists in Sri Lanka, agrees Consultant Obstetrician and Gynaecologist, Dr. Dhammike Silva who is also a Senior Lecturer at the Medical Faculty of the Sri Jayewardenepura Hospital, when prodded by the Sunday Times.
The team comprising Consultant Gynae-Oncosurgeon Dr. Chinthana Hapuachchi and Consultant Obstetricians and Gynaecologists Dr. Silva and Dr. Madura Jayawardane has taken laparoscopic procedures to a new height, nay amazing depth, in Sri Lanka.
There is not a hint of arrogance, only a matter-of-fact explanation as they describe how with clearer vision being the advantage of laparoscopy, they delved deep into “a very, very dangerous area” behind the aorta (the largest artery in the body) and the inferior vena cava (the largest vein), to grasp the lymph-nodes and pull them out in a clearance up to the renal vein.
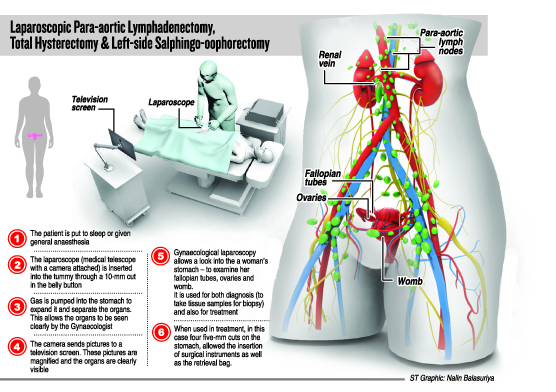
And the tongue-twisting procedure performed on October 28, was a Laparoscopic ‘Para-aortic Lymphadenectomy’ along with a ‘Total Hysterectomy’ and a ‘Left-side Salphingo-oophorectomy’.
The procedure entailed the removal of the para-aortic lymph-nodes, the womb (uterus), the left ovary and the left fallopian tube, the Sunday Times learns. (The para-aortic lymph-nodes are small bean-shaped tissues located near the aorta, right in front of several lumbar vertebrae.)
For this ‘more targeted clearance’, the team used five ports instead of three unlike in the usual laparoscopic procedures, with the camera being sent in through a 10-millimetre cut and the instruments through five-mm cuts. The cleared stuff was collected in a laparoscopic retrieval bag.
 “This patient came to us with fertility wishes,” explains Dr. Silva and a routine ultrasound scan sadly revealed a large mass on the right ovary.
“This patient came to us with fertility wishes,” explains Dr. Silva and a routine ultrasound scan sadly revealed a large mass on the right ovary.
Adds Dr. Jayawardane, that immediately there was a suspicion of cancer (malignancy). “Generally if there are suspicions, the usual practice is to take out not only the affected ovary but also the other ovary and the womb.”
However, because the couple was yearning for a baby, the doctors took out the ovarian mass which was about 12X15cm initially in open surgery, along with the right ovary and the right fallopian tube, it is learnt.
When the histopathology tests confirmed malignancy, intense were the discussions among the two Gynaecologists and Dr. Hapuachchi taking into consideration Kumari’s age.
“She was in her forties and unlikely to conceive. In-vitro fertilization (IVF) or a test-tube baby also seemed out of the question due to their circumstances in life. They simply could not afford IVF which is quite expensive,” says Dr. Silva.
Kumari is a garment factory worker and her husband a mason, the Sunday Times found on interviewing them over the phone.
There followed the three-doctor consensus that “total clearance” of the womb, left ovary, left fallopian tube and para-aortic lymph-nodes would be the safest action, in the best interests of Kumari.
When asked how the patient had not realised the cancer growing within her, Dr. Silva points out that in this particular area, the tumour has a large space to grow without the manifestation of symptoms.
“She would experience no major problems until the tumour grew large and began pressing against adjacent organs. Normally there would only be non-specific symptoms such as stomach bloating, regurgitation, constipation and backache. This is why ovarian tumours are usually detected late with disastrous consequences,” he stressed.
He urged women to get themselves checked thoroughly even if they experienced such non-specific symptoms as it would be better to be safe than have regrets later.
“The tumour was in the early stages,” points out Dr. Jayawardane, adding that it was also important to ascertain whether it had spread to the para-aortic lymph-nodes. For, if the lymph-nodes were affected by the malignancy, then chemotherapy would necessarily have to be given. Chemotherapy would bring with it other issues such as weight loss, hair loss and feeling ill.
However, if the para-aortic lymph-nodes tested negative for cancer, there would be no need for chemotherapy. This is why a para-aortic lymph-node dissection was important, added Dr. Jayawardane.
The team also decided to ‘de-bulk’ the area to prevent pressure from building up and causing potential problems, it is learnt.
“If in case the para-aortic lymph-nodes turned out to be malignant when tested and she needed chemotherapy, the de-bulking of the area would make chemotherapy more effective with smaller doses,” says Dr. Silva.
Back at home with her husband, Kumari* sans the cancerous mass which otherwise would have spelt a death sentence for her says that not only the doctors but also the nursing staff went beyond their call of duty in looking after her.
Happy that after the procedure there has been no pain at all, her humble tribute to these pioneering doctors is that she is “very proud” of them.
(*Name changed to protect the patient’s identity)
| Laparoscopy vs laparotomyThe major differences between a laparotomy (open surgery) and laparoscopy are: - Minimal blood loss - Less adhesions - Quicker recovery - Faster return to normalcy - Far better cosmetic result externally Unstinting support from Director The Obstetrics and Gynaecology Professorial Unit of the Kalubowila Hospital has developed highly-skilled laparoscopic procedures to a fine art. |

