News
Joy at the end of gruelling battle between life and death

A part of the team who put their shoulder to the ‘ECMO wheel’ to save Sunil’s life, get a photo with him when he arrives at the Cardio-thoracic clinic on Tuesday. Many are behind the scene.
Over the moon……not only the COVID-19 recovered patient but the Karapitiya Teaching Hospital’s ECMO team!
Off the ventilator, but still on ECMO (extracorporeal membrane oxygenation) after passing through a touch-and-go time, the video call from the hospital bed by this 39-year-old Merchant Navy officer was to his beloved wife and precious 10-month-old son.
It is from Sunil* now back at home after battling COVID-19 with the immense support of ECMO that we hear how he went to Colombo from Galle in July. That was to get the first dose of the vaccination, but by that time he had already been infected by the COVID-19 virus.
“Amaruwuna,” says Sunil, as body aches and pains engulfed him along with a slight cough. He consulted a doctor who gave him some medication but advised him that if he felt no better in two days, to get a test done for COVID-19. This is what he did on July 24 – a Rapid Antigen Test (RAT) which was positive.
 He then got admitted to a private facility in Galle but his health deteriorated, while at home too, the situation was not good. His wife, baby son, father-in-law, mother-in-law and brother-in-law had all been hit by the rampaging virus.
He then got admitted to a private facility in Galle but his health deteriorated, while at home too, the situation was not good. His wife, baby son, father-in-law, mother-in-law and brother-in-law had all been hit by the rampaging virus.
When he became “godakmaamaru” (critically ill) on July 25, he was transferred to the Karapitiya Teaching Hospital and within a short span of six hours “sihiyanethiwuna” (lost consciousness), coming to only on August 5 “hondawela” (recovered).
He had lost track of time but the doctors were by his side and connected him with his wife through a video call.
Pulled back from the brink of death, Sunil was fit enough to be discharged from hospital only on August 21, nearly a month after the Karapitiya ECMO team headed by Consultant Cardiothoracic Surgeon Dr. Tolusha Harischandra and Coordinator Dr. Kapilani Withanaarachchi who is also a Consultant Paediatrician had battled the ravages caused by COVID-19.
“The few COVID-19 patients who were referred to us earlier were not only ‘really sick’ but also brought in very late,” says Dr. Harischandra, stressing that if the lungs are irreversibly affected and there is multi-organ failure, there is nothing that can be done.
Dr. Withanaarachchi recalls how within 12 hours of being admitted to Karapitiya, Sunil had to be intubated (a tube had to be inserted into his trachea in an invasive procedure), as he needed ventilator-support to breathe. He was already on non-invasive ventilation (NIV) through a mask but that was inadequate to keep him alive.
The call for ECMO came very fast, within four hours, as even with ventilation his oxygen saturation was in the 70s, way below the required level of the 90s. To aggravate matters and cause worry lines for the doctors, Sunil’s blood sugar was also playing up and very high.

Perfusionist Buddhika setting up the ECMO circuit incorporating the cytokine adsorption cartridge
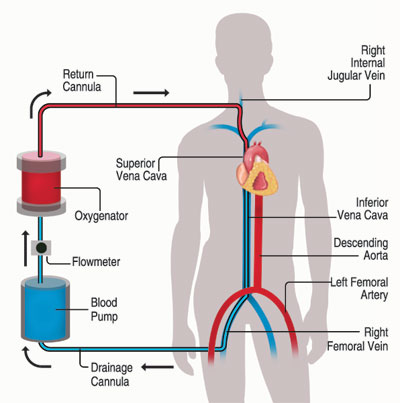
It was on the evening of July 26 that Sunil was given life support through ECMO which uses a pump to circulate blood through an artificial lung and send it back into the bloodstream, providing heart-lung bypass support outside the body.
Delving into the procedure, Dr. Harischandra says that they used the V-V ECMO (veno-venous ECMO) to support Sunil’s lung functions which were beleaguered by COVID pneumonia.
Sunil was attached to the ECMO apparatus by inserting one cannula into his Superior Vena Cava (SFC) through the right Internal Jugular Vein in the neck and the other into the Inferior Vena Cava (IVC) through the right Femoral Vein in the thigh.
The SVC is a major vein in the upper body which carries de-oxygenated or venous blood from the head, neck, upper chest and arms to the heart to be oxygenated. The IVC, considered a great vessel, drains de-oxygenated blood from the lower trunk, abdomen, pelvis and lower limbs to the heart for oxygenation.
Making it sound simple, Dr. Harsichandra says that the ECMO machine drained blood without oxygen from the IVC, pumped it through the membrane where carbon dioxide was removed and oxygen was added and then pumped this blood back into the SVC.
“There was also something special and different done to save Sunil’s life,” she says, pointing out that a ‘CytoSorb adsorber’ cartridge was fixed to the external ECMO circuit to reduce inflammatory mediators in the blood.
COVID-19 severe disease lets loose what is called a ‘cytokine storm’ that could otherwise lead to uncontrolled systemic inflammation, organ failure and death. (A ‘cytokine storm’ is a severe immune reaction in which the body releases too many cytokines into the blood too quickly. Cytokines play an important role in normal immune responses, but having a large amount of them released in the body in one go can be harmful.)
It was the first time that in ECMO therapy in Sri Lanka such an adsorber had been used.
However, there were also many other challenges the team continued to face as they kept Sunil on ECMO for eight days and Dr. Withanaarachchi talks of the struggle with infections that were wracking his body.
“He came with the infections and we managed them with antibiotics while a candida fungal infection in his urinary tract we dealt with through anti-fungal medication,” she says, also referring to the administration of heparin, a blood thinner.
It was a fine balance with heparin they had to maintain, not allowing bleeding into the brain while also preventing the formation of blood clots. Such clots would have been disastrous as they would have halted the functioning of the ECMO machine.

The team performing the ECMO procedures
Dr. Withanaarachchi explains how they have to get it “absolutely right”, as heparin is an integral part of running ECMO.
Pointing out that other major problems with patients in the Intensive Care Unit (ICU) are secondary infections caused by all the tubes snaking out of a severely ill person and all the drugs administered, she says that they were “very worried”. As soon as his lungs showed an improvement, they took him off the endotracheal tube and the ventilator.
With Sunil being conscious and able to talk, it was Awake ECMO thereafter with an RT-PCR test indicating that he was negative by that time.

Talking to the patient when he was on Awake ECMO
All this while some of the other challenges for the team had been working in Personal Protective Equipment (PPE) throughout,“a very difficult task” and performing procedures on the patient, while making sure that team members did not contract COVID-19. Another fearful thought was whether they would take the virus back to their homes and families.
An “emotional” day was August 5 when the cannulae were removed, separating Sunil from the ECMO machine, with steady progress on the road to recovery and discharge from hospital on August 21.
Dr. Harischandra and Dr. Withanaarachchi are ever appreciative of everyone – “a huge team” including doctors, perfusionists, nurses, para-medical personnel and healthcare assistants – who put their shoulder to the “ECMO wheel” to save Sunil.
From across the seas in the United Kingdom, there was guidance and support from Dr. Richard Firmin who had helped to introduce ECMO at the Karapitiya Hospital a while back, amidst many a challenge.
All those sleepless nights when they hovered over Sunil and stayed away from their families were fully worth it, says Dr. Harischandra, adding: “We cracked the code on how to save severely ill COVID-19 patients through ECMO.”
(*Name changed to protect identity)
| ECMO is not for them ECMO is not for all, the team has learnt through bitter experience – for Sunil is just one of four who survived. Currently, a doctor is on ECMO. After poring over literature and also taking into account the Karapitiya team’s experiences, Cardiothoracic Surgeon Dr. Tolusha Harischandra talks of the “ideal” candidates for ECMO in saving COVID-hit lives. These candidates are those with severe COVID-pneumonia which has not been responsive to the maximum conventional treatment.
| |

