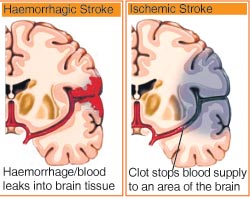
A stroke is a “brain attack” that happens when a part of the brain experiences a problem with blood flow. This disruption in blood flow cuts off the supply of oxygen to the cells in that part of the brain, and these cells begin to die. Damage to the brain can cause loss of speech, vision, or movement in an arm or leg, depending on the part of the brain that is affected.
Stroke is the major form of Cerebrovascular Disease, or CVD, a term that sometimes is used interchangeably with stroke.
Different strokes and their treatments
If the stroke is caused by a blood clot (ischemia), then thrombolytics (TPA - Tissue Plasminogen Activator) within three hours of stroke onset gives the best chance of recovery.
If the stroke is caused by bleeding (haemorrhage), then thrombolytics will worsen the condition, so the correct diagnosis is required before proceeding to medical treatment.
In other circumstances, doctors prescribe blood thinners such as heparin and Coumadin to treat strokes due to blood clots. Aspirin may also be used.
The physiotherapist’s role
Physiotherapists rehabilitate the patient with different techniques. They also teach home exercise programmes after the patient makes a considerable recovery. Physiotherapists check which muscles still have some power and check whether the patient is utilizing that muscle in functional movement and if not, teach him/ her how to use it.
If the patient is already using that muscle, then they try to improve the patient’s quality of movement and include voluntary control exercise in their treatment. If necessary, they ask the patient to have a proper splint for a lower limb if involved.
They also check the patient’s daily activities and needs and recommend different tasks for them. Aerobic exercise is included to increase the patient’s endurance for it improves cognition and perception if affected. Physiotherapists identify a recreational activity that would appeal to the patient. Posture awareness training and gait training are also emphasized.
Physical therapy
In stroke literature, the most important question is recovery or compensation. Recovery after stroke always depends on the area of brain involvement, size of lesion, duration of getting treatment and many other factors.
Some patients have complete recovery within a month and go on to live as normal. Full recovery without any residual dysfunction might be also because they might have only suffered from hemiparesis but this might not be the case with hemiplegia.
In other cases where the damage is greater, physiotherapists help patients to recover through a rehabilitation process with all other drugs and medications. They train affected muscles through strengthening, stretching, PNF (Proprioceptive Neuromuscular Facilitation), and other treatments to gain the maximum level of independence. During this period, the patient’s brain learns to do the activity near normally without use of the infarcted part of brain. In other words, the normal part takes over the function of the infarcted part, so that the patient can recover near normal movement without any dependence.
Lesion location and all other things described above play a huge role in gaining recovery.
But in chronic stages also, now it is believed that neural plasticity (i.e., the surrounding neurons branch to the affected area and try to provide collateral circuit to optimize function) does occur and so based on that true recovery of such chronic patients is possible. With appropriate physical therapy and practice, there are chances of gaining true recovery in chronic stroke patients too but it would still differ from patient to patient.
Still a question remains of how much true recovery can be expected from chronic stroke patients but there is a hope that in about 10-15 years, the rehabilitation of such stroke patients might be completely different.
Common PT techniques used in stroke rehabilitation
- Proprioceptive Neuromuscular Facilitation (PNF)
- Neuro Developmental Technique (NDT)
- Bobath’s Technique
- Rood’s approach
General PT caring tips
1. Maintain and improve the mobility of affected limbs
- Patients are encouraged to use their affected limbs.
- Patients should do limb exercise properly according to the physiotherapist’s instruction.
2. Increase the awareness of affected limbs
- Try to approach the patient on the affected side during feeding, conversation or transfer. Then the patient could be assisted more effectively. Besides, it could improve awareness of the affected limbs so as to stimulate the patient’s usage of the affected limbs.
- Place daily necessities next to the affected side.
3. Prevent injury
- Use walking aids (e.g. stick, quadripod and walking frame) and wheelchair properly according to physiotherapist’s instruction.
- Wear suitable footwear so as to prevent foot injury and falls.
- Avoid placing objects which are too hot, too cold or sharp near the affected side.
4. Adopt proper posture
- Adopt proper posture in the following so as to prevent increase of spasticity.
- In lying position
- Use a firm mattress, approximately 5 cm thick to provide adequate support to the spine and the affected limbs
- Use a firm pillow with a suitable thickness so as to give good support to the neck. The head should be in horizontal alignment with the trunk and the neck should not be bent or dropped backward.
- If necessary, support the affected limbs in relaxed position with 3-4 pillows, with the elbow and fingers straightened and the knee slightly bent.
- Turn the patient into different positions every two hours if the patient cannot move on his/her own.
- In sitting position
‑ Choose a suitable chair with backrest, arm rest and firm seat to provide good support.
- Support the affected upper limb with a pillow or armrest, with the elbow and fingers straightened.
- The depth of the seat should be appropriate so that the patient can sit straight with his/her back supported by the backrest.
- The height of the chair should be appropriate so that the patient’s feet can be placed on the floor comfortably, with the hip and knee flexed at 90 degrees.
5. Care of limb swelling
- If required, wear elastic stockings on the affected limbs and apply passive exercises to the limbs according to the health professional's instruction.
- Support the affected limbs in an elevated position when resting.
6. Maintain good personal hygiene
- Observe good personal hygiene.
- Keep the web spaces and joint lines of fingers and toes clean and dry in order to prevent odour and skin disease.
7. Adopt proper lifting and transferring technique
- Patients should adopt proper transferring technique to prevent worsening of spasticity of affected limbs. For example:
- Don’t pull the rail of the bed to be upright from a lying down position,
- Don’t only place weight on the unaffected leg in transferring or standing, etc
- Caregivers should assist patients, whenever necessary, by using proper lifting and transferring techniques
- Hold the patient firmly without pulling the affected upper limb to avoid causing injury to the limb.
- Caregivers should maintain a proper posture by keeping close to the patients, the back straight and knees bent during the transfer process so as to prevent back injury.
(The writer is Chief Physiotherapist, Motivation Charitable Trust Sri Lanka)
|