Let’s talk endometriosis
View(s):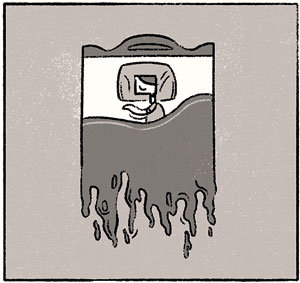 Vraie Balthazar remembers thinking: “This can’t be normal.”
Vraie Balthazar remembers thinking: “This can’t be normal.”
Her periods had taken on a kind of life of their own. She would bleed not just three or four days, but seven days. Her sanitary napkins needed to be changed every two hours. She would layer them together, two-pads deep, to make a kind of adult diaper; even then it wasn’t enough. She stopped wearing white.
Before she went to sleep, she would set her alarm for 3.30 a.m., so that she could get up and change her pads. But her mattress got stained so many times anyway that she took to sleeping on a plastic sheet. And there was the debilitating pain: she had headaches and joint aches that got progressively worse and left her unable to function.
Yet, the first time she went to a doctor, he told her that her flow was regular, and sent her home. It would be a long time before she returned to a gynaecologist, and several years before she had a name for her condition: endometriosis.
 A misunderstood condition
A misunderstood condition
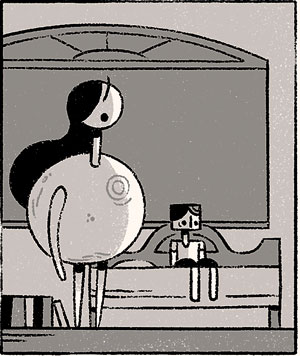
When we meet Dr. Himani Molligoda, a Consultant Obstetrician and Gynaecologist, she has coincidentally just seen a patient who has endometriosis. In this young girl the condition has manifested differently – blood has filled her ovaries, turning them into a small balloon. Dr.Molligoda’s patient came looking for help after she fainted three times from the pain and utter exhaustion.
“This is one of the most difficult and challenging conditions for us to treat,” Dr. Molligoda says frankly. She points out that the symptoms can vary dramatically and the causes of endometriosis aren’t fully understood. What is known is that the gynaecological condition occurs when tissue similar to the lining of the womb is found in other areas of the body, including the ovaries, fallopian tubes, pelvis, bowel, vagina and intestines.
 During a woman’s menstrual cycle, her body releases hormones that make the lining of the uterus thicker. If she does not become pregnant, this lining falls away, and along with blood is ushered out through the vagina. In women with endometriosis, the cells from the womb that are now outside will also swell and then fall away. In the process, they can damage organs they are in contact with, cause internal bleeding and leave behind scarring. In some cases they cause organs to stick together, creating all kinds of complications which could require serious surgery.
During a woman’s menstrual cycle, her body releases hormones that make the lining of the uterus thicker. If she does not become pregnant, this lining falls away, and along with blood is ushered out through the vagina. In women with endometriosis, the cells from the womb that are now outside will also swell and then fall away. In the process, they can damage organs they are in contact with, cause internal bleeding and leave behind scarring. In some cases they cause organs to stick together, creating all kinds of complications which could require serious surgery.
There is no known cure for the condition, says Dr. Molligoda, but helping women stay largely period-free can help ease the symptoms. However, many patients do not even realise that they have the condition in the first place.
As a young girl growing up in Colombo, Sulakshana Perera* didn’t realise she was experiencing something out of the ordinary. “I would try to hold up, but I was completely exhausted, and there were days I couldn’t stand. My legs would hurt, and my hips too, as if someone had whacked me with a ton of bricks.”
By the time she got to university, the pain had become so much worse. Her friends and family, though sympathetic, thought she was only going through what all women go through – what was all the fuss about?
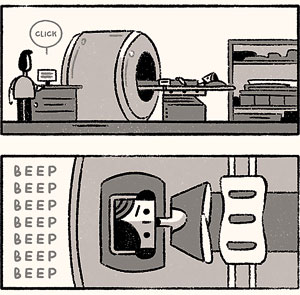
 “There were these days when I just could not get out of bed. I would be crying in pain, and throwing up,” she remembers, adding that these extreme symptoms finally got her to a doctor. She should have had a scan, but the consultant suggested she do a blood test – the results didn’t seem particularly serious, and so Sulakshana’s experience was brushed aside: she was told it might be a muscle issue; two Panadols would take care of it. But that didn’t explain why the pain coincided with her period every month, and the pain itself simply just wouldn’t go away.
“There were these days when I just could not get out of bed. I would be crying in pain, and throwing up,” she remembers, adding that these extreme symptoms finally got her to a doctor. She should have had a scan, but the consultant suggested she do a blood test – the results didn’t seem particularly serious, and so Sulakshana’s experience was brushed aside: she was told it might be a muscle issue; two Panadols would take care of it. But that didn’t explain why the pain coincided with her period every month, and the pain itself simply just wouldn’t go away.
The question of fertility
When Sulakshana finally got a diagnosis of endometriosis, it came with some bad news. One of her ovaries had been irreversibly damaged, and it could affect her chances of having a child. The first consultant she saw wanted this young woman to immediately marry and have a child. Sulakshana was aghast – it was not that she was against either marriage or children in principle, but it seemed like an absurd reason to tie the knot.
She found another consultant who prescribed birth control tablets. Sulakshana found that taking it regularly reduced her symptoms dramatically. But as a single woman, buying the pill wasn’t always easy. At the counter, judgmental pharmacists would sometimes refuse to sell it to her. At home, she remembers a close relative telling her dismissively that she should be worried about putting on weight and should get off birth control. Sulakshana burst into tears of pure frustration – “I was in so much pain,” she told her aunt, “this is the only thing that helps.” Thanks to such experiences, Sulakshana seldom spoke of her condition.
Meanwhile, Vraie too was being given advice not to discuss her diagnosis with anyone. Since endometriosis is known to impact fertility, she was told it was best she hide it from everyone. However, her husband proved to be her most faithful champion, and went on every doctor’s visit with her. After trying for many months, they had their first child, and then a second.
“It took a while and the waiting felt horrible,” recalls Vraie, adding, “women are told that we are these vessels that are meant to carry children, and that if there is something wrong in our bodies, it is our fault, and we are to blame. It’s so very unfair.” Even doctors sometimes did not take women’s complaints of pain and bleeding seriously – leaving people to move from one consultant to the next, always in pain and trying to hide their condition from people around them.
 This is particularly true for women of marriageable age in Sri Lanka, says Vraie. “I feel guilty,” she admits, “I have these two beautiful children, and so now I am able to be more open about it. I don’t know if I would have spoken out if we didn’t already have a family.” In the years since the birth of her daughter, Vraie has become increasingly vocal, convinced that women should be able to have frank discussions about something that affects them so deeply.
This is particularly true for women of marriageable age in Sri Lanka, says Vraie. “I feel guilty,” she admits, “I have these two beautiful children, and so now I am able to be more open about it. I don’t know if I would have spoken out if we didn’t already have a family.” In the years since the birth of her daughter, Vraie has become increasingly vocal, convinced that women should be able to have frank discussions about something that affects them so deeply.
Dr. Molligoda agrees. She’s seen women who spend the entire month in pain, or completely debilitated by the condition, and says its critical not only that people seek help if they suspect something is wrong, but also that they stay on a treatment regimen, taking the time to really understand what is happening with their bodies. Surgery is not inevitable, she emphasises. However, neglecting the condition cannot only devastate women’s health, it can also result in deep depression and stress.
For her part, Vraie thinks women should talk to each other more. Posts on her Facebook page, in which she is honest and open about the condition, have inspired a strong response. “I don’t ‘look sick’,” she writes, “so there’s a constant misconception, even amongst family and friends, that it can’t be ‘that bad’.”
For every woman who posts a comment in response, another three send her a private message – an indication of how many women are struggling to cope in secret. Vraie says she hopes to see the stigma lessen, after all discussing menstruation shouldn’t be taboo or distasteful. When we treat it as such, it becomes harder for women to seek the help they need. “We shouldn’t be afraid to talk about our bodies, our periods or being ill,” says Vraie.
*name changed to protect privacy
(The images in this article are courtesy Isuri M. H., from her comic 3x3x3 which depicts her own experiences with endometriosis. For the full comic, visit: https://artofisuri.com/3x3x3)


