After ERAS, mERAS brings honour to Sri Lanka
Bowel cancer, surgery and management the traditional way have been inextricably linked in Sri Lanka, until a bright young surgeon returned in 2010 from the United Kingdom (UK) and turned this thinking upside down.
 Breaking free of tradition, he introduced laparoscopy (keyhole) or minimal-access surgery for colorectal cancers as well as the “revolutionary” management of patients both before (pre) and after (post) surgery.
Breaking free of tradition, he introduced laparoscopy (keyhole) or minimal-access surgery for colorectal cancers as well as the “revolutionary” management of patients both before (pre) and after (post) surgery.
It provided huge relief to the patients and did not entail keeping him/her starving for the bowel to heal.
It is this same surgeon who has now moved a major step forward, adapting the treatment of bowel cancer, from a rich-country setting to suit resource-poor settings like Sri Lanka.
In the process, he and his team have brought honour to Sri Lanka by winning the prestigious Surgical Team of the Year award at the BMJ Awards South Asia 2018 held in December in Chennai, India, competing with many others from the region.
As many as 1,575 high-impact projects in various spheres of health from the nine countries of Afghanistan, Bangladesh, Bhutan, India, the Maldives, Myanmar, Nepal, Pakistan and Sri Lanka had vied for the awards under 10 categories. Competing with a powerful contender such as the All India Medical Institute in the final-round, the Sri Lankan team has been able to walk off with the award.
The team from Sri Lanka was headed by Consultant Surgeon Dr. Bawantha Gamage of the Colombo South (Kalubowila) Teaching Hospital and Head of the Department of Surgery, Faculty of Medical Sciences of the University of Sri Jayewardenepura.
A modified enhanced recovery after colorectal surgery (mERAS) is what won them this important award earning peer-praise. Back in 2010, he first introduced ERAS to Sri Lanka.
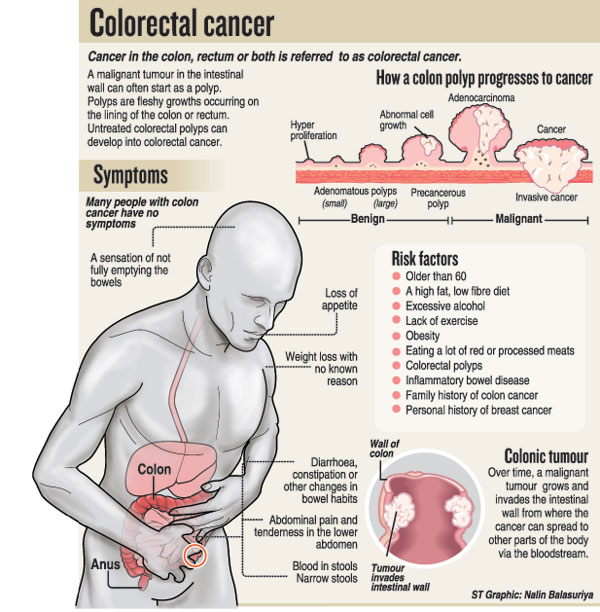
Before MediScene gets down to the details of the latest achievement in the form of mERAS, Dr. Gamage says that it has become the gold standard in the management of colorectal cancer, the fourth most common cancer in Sri Lanka.
The benefits of mERAS are early mobilization, reduced hospital stay and lower mortality (deaths). A study by the team has found that the 30-day mortality of those who undergo mERAS is zero, MediScene learns.
 ERAS by itself was a first in Sri Lanka, when Dr. Gamage returned after extensive training in laparoscopic colorectal surgery at the Colchester University Hospital in the UK.
ERAS by itself was a first in Sri Lanka, when Dr. Gamage returned after extensive training in laparoscopic colorectal surgery at the Colchester University Hospital in the UK.
Traditionally, patients who have cancer in the rectum or colon and have to undergo surgery – either open or laparoscopic — get a thorough bowel clean-up with medication, while being given plenty of fluids, with polyethylene glycol usually being taken before the operation. After the operation, these patients are kept fasting for three to four days, with lots of fluids being administered intravenously.
However, it had been found that the ‘traditional protocol’ delayed patient recovery, with there being a fluid overload. Cleaning the bowel thoroughly, meanwhile, caused it to go into paralysis due to an electrolyte imbalance. This delayed bowel function.
The assumption under the traditional protocol was also that giving food to the patient soon after the operation would impair the healing of the joint which had been sutured together after the malignant part was excised (removed) and may lead to leaking.
ERAS, however, changed all that — instead of the traditional bowel-clearing medicine, for patients who have to undergo surgery for left-side colon and rectal surgery, only an enema was given on the morning of surgery. No pre-op bowel preparation was done in those who had to undergo surgery for right side colon cancer, explains Dr. Gamage.
Post-op too, the situation changed and the patient was not starved, but given liquids soon after the anaesthesia wore off. Later, the patient was allowed to consume solid food.
Now comes mERAS, with more advantages for those who have to undergo surgery for colorectal cancer.

Dr. Bawantha Gamage (second from right) with his award
| Advantages of laparoscopic (keyhole) surgery The Colombo South (Kalubowila) Hospital has since 2010, performed laparoscopic (keyhole) surgery for colorectal cancer, also believed to be a first in the country. Here too the advantages are many, according to Dr. Bawantha Gamage. The advantages in laparoscopic surgery as opposed to open surgery for colorectal cancer are: Under traditional surgery, there is a 10-inch midline cut on the patient’s abdomen but in laparoscopic surgery there are only four small incisions (cuts). These are the five-mm cuts for the laparoscope (camera) and the two instruments that Dr. Gamage handles and a 12-mm cut for the bowel-joining stapler. In open surgery, the surgeon’s eye and the operation site are as far as 12 inches or more. But in laparoscopic surgery, there is enlarged vision for the surgeon, as his eye is at the tip of the camera-lens, just 3-4 cm away at the tip of the telescope. As such, he has a magnified, high-definition view of the operation site on the monitor which allows for easy identification of the fine structures in the abdomen. There is also much handling of the bowel in open surgery, but in laparoscopic surgery, the patient is positioned in such a way that his/her head is 45 degrees inclined downward and the bowel moves in that direction automatically. This is using gravity as a force of retraction to move the bowel away from the pelvis. So the surgeon has good access and everything gets back to the normal position after the procedure, quickening faster recovery of the bowel. In the laparoscopic procedure, there is less blood loss, less pain and fewer days in hospital. Success story Referring to the “success story” of an evidence-based paradigm shift, Dr. Bawantha Gamage contrasts the modified-ERAS (mERAS) with the standard ERAS protocol. The patient is admitted to hospital, the day before surgery in mERAS, while the admission is on the same day for ERAS. Intra-operative central venous pressure guided fluid therapy in mERAS, while under ERAS it is intra-operative non-invasive goal directed fluid therapy. Selective use of drains in patients who have undergone anterior resection (removal of a part of the rectum), total proctocolectomy (removal of the colon and the rectum) and abdominoperineal resection (removal of the entire rectum and anal canal), with a nasogastric (NG) tube used to establish feeding in mERAS. Under ERAS, no drains and NG tubes are recommended. Overnight Intensive Care Unit (ICU) management given in the first 24 hours under mERAS as the hospital did not have High Dependency Unit care initially. Post-op routine ICU care not recommended under ERAS. Discharge of patient after establishing a normal diet and mobility (5-6 days) under mERAS due to lack of adequate outreach patient care in Sri Lanka. Under ERAS, early discharge (3-5 days) from the hospital. “On my return after training in the UK, I wanted to establish a sustainable ERAS protocol that is suitable to a developing country such as Sri Lanka. However, all steps were not possible due to resource limitations and this is why we have come up with the mERAS protocol,” says Dr. Gamage. | |


