When it is more than just a tummy ache
Many of us have experienced a “tummy ache” at some point in our lives. Depending on the severity and the circumstances we tend to respond in different ways. Some take paracetomol, some swear by antacids and yet some others take nothing. Often these tummy aches tend to subside after some time and they are later commonly referred to as “gastritis.” However there are situations where these tummy aches are more serious and when associated with other features mandate medical/surgical opinion.
Dr. Imtiaz Ismail
What features suggest that this is
no simple tummy ache?
Severe or persistent pain
Fever
Vomiting
Increasing abdominal girth
Blood stained stool or vomitus.
Blood stained urine/painful urination
Inability to open bowel or pass gas.
Letharginess/unresponsiveness.
In a female heavy or irregular periods
Common causes for abdominal pains
Non-specific
Appendicitis
Gallstones/cholecystitis
Peptic ulcer complications
Pancreatitis
Kidney and bladder stones
Bowel obstruction
Blood vessel pathology-aortic aneurysm, mesenteric ischemia
Gynaecological conditions-Ectopic pregnancy, Twisted ovarian cyst
Miscellaneous-Dengue, bowel and renal infections, bleeding disorders, Mesenteric adenitis, etc..
 The above list is by no means exhaustive but only includes some of the more common/important causes of abdominal pain. We will briefly discuss some of the conditions which present in a surgical casualty ward.
The above list is by no means exhaustive but only includes some of the more common/important causes of abdominal pain. We will briefly discuss some of the conditions which present in a surgical casualty ward.
Non-specific abdominal pain
Every patient admitted to a hospital does not get a diagnosis such as appendicitis or a renal infection. Such abdominal pain lasting less than 7 days and with negative routine examination and baseline investigations are labelled non-specific. It is estimated that this accounts for nearly 35% of all abdominal pain. The physician usually adopts a “wait and see” policy.
 Appendicitis
Appendicitis
-Commonest acute surgical abdominal emergency
-Common age-Early teens, late 40’s
-In the USA more than 250,000 appendicectomies are done per year.
Symptoms-
Initially central abdominal pain later localizing to right lower abdomen. Associated with nausea and/or vomiting.
Diagnosis-
Often an experienced surgeon will diagnose this by merely placing his/her hand on the patient’s abdomen.
Routine blood tests and sometimes an abdominal scan may be required.

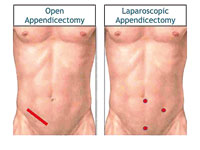
Laparoscopic cholecystectomy
Treatment-
The treatment of uncomplicated appendicitis is Appendicectomy. This may be open or laparoscopic{keyhole}
Cholecystitis
This is inflammation of the gallbladder commonly due to obstruction of the cystic duct by gallstones which form in the gallbladder.
10% of cases are due to causes other than gallstones. 2-3 times commoner in females. In the USA about 600,000 cholecystectomies (gallbladder removal)are performed annually.
Symptoms
Upper central/right upper quadrant pain which may radiate to right shoulder or shoulder blade. Initially colicky, later almost always constant. May have nausea, vomiting and rarely jaundice.

Open cholecystectomy
Investigations
Blood tests
Ultasound scan is the best and most readily available imaging test
CT/MRI – secondary imaging modalities
Treatment
Requires hospitalisation with IV antibiotics, pain relief and careful monitoring. The definitive treatment of uncomplicated cholecystitis would be cholecystectomy which may be open or laparoscopic.
Peptic ulcer complications
Peptic ulcers refer to defects in the mucosa of the stomach (gastric) or small bowel (duodenal) that extend to a certain layer (muscularis mucosae) In the United States, peptic ulcer disease (PUD) affects approximately 4.5 million people annually. Approximately 10% of the US population has evidence of a duodenal ulcer at some time.
Incidence of peptic ulcers increase with age. Males and females are equally affected.
Strongly associated factors include Helicobacter-pylori (Bacteria),non-steroidal anti-inflammatory drugs and smoking. With H-Pylori eradication therapy the worldwide incidence of ulcer disease is diminishing. Complications of peptic ulcer include bleeding, perforation, and malignant change.

Gastric ulcer
Symptoms of perforation
Sudden severe pain upper/central abdomen associated with sweating. May have vomiting which may be blood stained. Some may present even in a collapsed state.
Diagnosis of perforation
Along with above clinical features and careful examination, useful investigations are Blood tests, Chest X-Ray, Abdominal scan and ideally a CT scan.
Treatment
Initally treated with IV fluids, antibiotics and proton pump inhibitors. Definitive treatment is emergency surgery which can be open or laparoscopic. Usually fatal if surgery is delayed. Recently in the UK where the best of facilities is available, a young lady whose peptic ulcer perforation was operated six days later, unfortunately died.

Bowel obstruction
Pancreatitis
This is inflammation of the pancreas and can present acutely or in a chronic manner with recurrent hospital admissions. Worldwide, the incidence of acute pancreatitis ranges between 5 and 80 per 100,000 population. Common causes are gallstones (40%) and alcohol (35%). Smoking is associated with both acute and chronic disease.
Symptoms
In the acute form presents with severe upper abdominal pain radiating to the back. May be associated with vomiting. In severe cases can present in a collapsed state.
Investigations
Blood tests – serum amylase and/or lipase.
Ultrasound scan
CT/MRI in certain clinical scenarios
Treatment
In the majority of patients, supportive therapy and rigorous monitoring is indicated. This may involve ICU management. Indications for surgical intervention include pus collections around the pancreas, pancreatic necrosis (destruction) and yellow discolouration of the eyes (Jaundice) due to gallstone impaction in the bile duct. The overall mortality in patients with acute pancreatitis is 10-15%. Patients with biliary pancreatitis tend to have a higher mortality than patients with alcoholic pancreatitis.
 Kidney and bladder stones
Kidney and bladder stones
This is very common in our country. Stones usually composed of either oxalate, phospate or uric acid. Commonest age group 30-50 years.
Symptoms
Some may be silent.
Pain- Maybe fixed loin pain or loin to groin pain
Blood stained urine maybe present
Investigations
X Ray/ Abdominal scan/CT Urogram
Treatment
Majority of stones pass spontaneously. A stone less than 4 mm in diameter has an 80% chance of spontaneous passage. This falls to 20% for stones larger than 8 mm in diameter.
Treatment modalities available include drugs such as Tamsulosin, Shock wave lithotripsy, Percutaneous nephrolithotomy and less commonly open surgery.
Bowel obstruction
This may affect both small as well as the large bowel. Causes include adhesions from previous surgery (60% of small bowel obstruction), internal or external hernia, cancers (Large bowel), twisted bowel (volvulus), hard stool, etc..
Symptoms
Small bowel- Central abdominal pain. May have vomiting. May be associated with an irreducible umbilical or groin hernia.
Large bowel- Present with inability to pass stool/gas
Gradual or sudden abdominal distention
May have vomiting
Investigation
Plain X Rays (Investigation of choice in SBO)
CT scan (Investigation of choice in LBO)
Small bowel/Large bowel endoscopy.
Treatment
Inital resuscitation with fluids and naso-gastric tube drainage. Some benign forms of obstruction such as adhesions may settle with this. Many will require surgery which depends on the site and type of obstruction, fitness of the patient, experience of the surgeon and the facilities available. Surgery includes resection of non-viable bowel, release of an obstructing band, resection of a cancer, repair of a hernia, etc.. Surgery may be open or laparoscopic.
Dengue
With the current dengue epidemic in the country, it is important to be aware that at times, in the leaky phase of the illness, abdominal pain may be a clinical feature. As surgeons, we are sometimes called upon to exclude appendicitis or other surgical events in these patients. Good clinical judgment and repeated evaluation along with appropriate investigations is required in assessing these patients.
(The writer is Consultant Surgeon, Colombo South Teaching Hospital, Kalubowila)


