Sunday Times 2
Minimising preventable deaths; critical care education is crucial
View(s):By Dr. Chula Goonasekera
 he impetus for the evolution of medicine in the world has always been the quest to improve patient survival and outcomes. In keeping with this paradigm, it is essential for a country to be on par with the rest of the world regarding recognition of its health care service and training. For example, cardiologists are preferred to general physicians in the event of a cardiac ailment. If a child is ill, we prefer a paediatrician and if it’s a neonate, a neonatologist to offer best advice and therapy. Imagine in this 21st century if we had no oncologists? Patients with cancer will have no hope for survival and our level of care would be at rock bottom in the world. Similarly, if we are critically ill, we need a critical care specialist. Sadly, we are yet to commence a full time critical care specialist training program in this country. Despite repeated requests by the Ministry of Health, the Post Graduate Institute of Medicine is yet to launch a dedicated critical care specialist training pathway that was promised in 2011 following the initiation of a diploma program. Further training of the critical care diploma holders has been blocked. Why are we so frightened of promoting critical care expert education? It will only lead to better cost effective health care and survival of more critically ill patients who would have otherwise perished. This article explains what critical care involves, and what we are losing as a country with this inexcusable delay in promoting the training and recruitment of full-time critical care specialists in our hospitals. Just think about the number of lives we could save, for example, due to dengue or after road trauma?
he impetus for the evolution of medicine in the world has always been the quest to improve patient survival and outcomes. In keeping with this paradigm, it is essential for a country to be on par with the rest of the world regarding recognition of its health care service and training. For example, cardiologists are preferred to general physicians in the event of a cardiac ailment. If a child is ill, we prefer a paediatrician and if it’s a neonate, a neonatologist to offer best advice and therapy. Imagine in this 21st century if we had no oncologists? Patients with cancer will have no hope for survival and our level of care would be at rock bottom in the world. Similarly, if we are critically ill, we need a critical care specialist. Sadly, we are yet to commence a full time critical care specialist training program in this country. Despite repeated requests by the Ministry of Health, the Post Graduate Institute of Medicine is yet to launch a dedicated critical care specialist training pathway that was promised in 2011 following the initiation of a diploma program. Further training of the critical care diploma holders has been blocked. Why are we so frightened of promoting critical care expert education? It will only lead to better cost effective health care and survival of more critically ill patients who would have otherwise perished. This article explains what critical care involves, and what we are losing as a country with this inexcusable delay in promoting the training and recruitment of full-time critical care specialists in our hospitals. Just think about the number of lives we could save, for example, due to dengue or after road trauma?
What is Critical Care Medicine?
Critical care medicine (CCM) is a modern independent speciality that has evolved from what was termed intensive care in the 20th century. Today, the role of critical care specialists is not limited to the confines of the intensive care units. They are now actively engaged across the board in hospitals in identifying clinically deteriorating patients through early warning by scoring systems long before they need intensive care. They initiate early corrective therapies that are appropriate to avert the need for admission to intensive care. Thus, they play a significant preventative role in managing critical illness. Early detection and averting deterioration is the most effective form of critical care therapy to ensure best outcomes. Critical care specialists are highly trained, like any other specialist such as a cardiologist, orthopaedic surgeon or an anaesthetist. Their main goal of therapy is to improve survival of patients, minimise their need for admission to intensive care and minimise the duration of stay in intensive care through safe, effective and efficient supportive care without aggravating organ damage. Therefore, the focus is patient centred and geared to fulfil the needs of the patient at the earliest opportunity and ensure their return to normal life with no residual damage. Critical care specialists work with critically ill patients, in collaboration with multiple specialists everywhere in the hospital.
Critical care medicine embodies more than a collection of treatments. It is a health care delivery process demanding especially skilled health care providers (critical care specialist doctors and nurses, physiotherapists, pharmacists, and so on) within an organizational framework that titrates often conflicting treatments, minimises potential treatment errors, and promotes the safe and efficient application of appropriate and timely care.
What is critical illness?
In a normal healthy state, we can compensate for injury or illness using our enormous reserve capacity. For example, if we hold our breath for one minute, it will not have any lasting effect on most of us, and we would just carry on as if nothing has happened. For a critically ill patient, this is no joke. Holding breath or losing breath for one minute could kill him or her instantly as he or she has no compensatory mechanism. A patient with heart failure needing continuous supportive medication would similarly succumb to the inevitable predicament of death if the infusions were blocked or disconnected for even a few seconds. Therefore, critically ill patients need very close continuous monitoring, with alarms to alert staff instantly if something goes wrong. The rectification of these issues should be instant. Therefore, there is a need for especially trained nurses and doctors to be resident at the bed side all the time, both day and night in critical care areas. Doctors and nurses with basic qualifications may not be able to expedite this standard of care needed to save lives. Thus, both nurses and doctors need additional competence based comprehensive training before managing critically ill patients. If we don’t have this degree of competence available at the bedside, it’s none other but patients who would suffer sometimes at the cost of their own lives. Losing a breadwinner of a family this way from a preventable cause is a tragedy, an unbearable loss to the family and the country. That is why we need to ensure that critical care services are improved to the highest possible standard in this country.
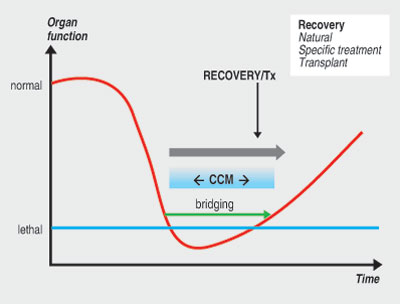
Critical illness arises when organ injury (whatever the cause), leads to organ failure. If we do not support the failing organ function, the situation turns lethal. For example, if our lungs are failing, we need to keep the patient oxygenated until this function recovers. If we cannot support lung function until recovery the result is inevitable death. Thus, critical care medicine is the bridge that maintains life in these grim circumstances of illness.
Losing confidence and trust
Despite modern advances in medicine, we are yet to install a dedicated training program to produce specialists to lead our critical care services. In the world, specialities have developed to enhance service to patients and improve outcomes. Sadly, this development path has taken a bumpy ride in Sri Lanka, since improving patient care and outcomes in critical care does not appear to have been the overriding goal in our establishment. A training path for this purpose was designed in 2008 by the Postgraduate Institute of Medicine, Colombo, the sole institution responsible for postgraduate medical training in this country, but this came to a halt halfway, with no further progress for the last eight years. The result is a gradual build-up of no confidence and distrust amongst our patients including that of our own politicians, doctors and nurses. This is reflected by the increasing number of our patients (including doctors) needing critical care opting to receive this modality of care, in our neighbouring countries like India, Singapore or even the more distant shores of the west at an exorbitant cost. Even the media is now openly seeking financial assistance and raising the necessary funds to assist patients receive such care abroad. Instead, what we should be doing is diverting our efforts to motivate our health care leaders, educators and government to promote standards of health care through training and the provision of facilities. The reasons for the lack of such safe and advanced treatment in this country should be explored and rectified. Recent mass protests against unexplained deaths in our hospitals should be considered as early warning signs of mounting mistrust amongst the public on our medical services. Sadly, innocent doctors and other health care workers have become targets of public anger and frustration. Regrettably, deaths of some of our eminent public leaders in our hospitals have also been the subject media critique in the recent past.
The duty
Today, in the developed world, critical care specialists undergo an independent comprehensive training program, including in our neighbouring country India. It is a specialty that is fundamental to support all other specialties to successfully implement their advanced therapies and therefore an essential catalyst to promote speciality advancement in this country. For example, there is no point embarking on a heart or liver transplant in this country if the critical care set-up is not up to the standard to deal with the supportive care they need. We need critical care specialist nurses and doctors all-round the country to help us save lives that would otherwise be sadly lost prematurely.
Critical care specialists should be committed fulltime to the critical care services and not overlook this whilst catering full-time to a major specialty such as anaesthesia or internal medicine. We must move away from this outdated model of practice prevalent in this country. Hybrid models such as these that place little emphasis on accountability and responsibility have introduced a dampening effect upon our advancement in medicine and this is already evident. The Ministry of Health should take the lead in creating critical care specialist cadre positions, at least in our regional hospitals with immediate effect so that a critical care service scenario can develop. Critical care specialists should dedicate their services full time to critical care and not be doing other specialty work such as anaesthesia full-time and hope moonlight visits to the intensive care unit are sufficient to improve patient outcomes. Our current intensive care mortality rates exceed 30% and sadly this is twofold higher than the norm. Thus, as many as 2/3rd of the deaths may be preventable. The excuses are aplenty in not wanting to evolve forward. However, two national institutions have a duty of care to achieve this milestone, i.e. the Ministry of Health and the Postgraduate Institute of Medicine as after all it’s the people who fund these institutions.
Acknowledgement: Mahes Salgado, the Head English Language Teaching Unit, University of Peradeniya
(The writer is a consultant anaesthetist based in London.)
email cgoonase@sltnet.lk

