The skies had opened up. The rains were heavy and continuous and there was flooding across the country. That Friday was particularly bad but the wrath of the weather gods did not deter them. Men and women, both young and old, braved the weather, gathering from afar at Ward 8 of the Sri Jayewardenepura General Hospital.
They came not only to meet those who had suffered a similar fate, gone through agony, unable to eat and sometimes even to take a large gulp of water, but also to say “thank you” to someone who had pulled them back from death’s door.
 |
| Seventy-year-old Ariyadasa |
He with the “gifted hands” had notched up a century and that too only at Sri Jayewardenepura without counting the numerous operations elsewhere even in Polonnaruwa (where the first operation had been done) at a time when the area was considered remote.
One after the other, they stood without inhibitions to speak of their experiences at the hands of Consultant Surgeon Dr. Gamini Goonetilleke since 1993 whose nimble and skilful fingers had given them a chance to enjoy a simple meal with relish. Something most of us take for granted.
They had come in their numbers to form a society
Ahara marga prashna (problems in the digestive tract), said the ever-grateful P.G. Ariyadasa from Polonnaruwa who had gone under the scalpel way back in 1994 and unfailingly comes with his gift of a humble pot of curd to see the doctor every three months so many years after.
For some, their digestive system so vital for human survival and well-being had started malfunctioning due to diseases but for others due to their own thoughtless actions of swallowing corrosive on the spur of the moment to regret in agony thereafter.
The problems were not restricted to the digestive tract but caused social, mental, personal and financial issues, MediScene understands. “I couldn’t swallow”; “I couldn’t eat”; “I couldn’t drink”; “I was vomiting all the time”……..were some of the many complaints they had come with. Some had been written off, with gangrene setting in parts of the digestive system, others had burnt or swollen gullets or stomachs and still others had a permanent tube stuck into their nose to enable liquid feeding.
Not any more. Having undergone major surgery to repair their systems they are leading normal lives and going about their work.
Referring to “these intense operations when we don’t even know that we are breathing”, Registrar Dr. Madhushanka Gomez says they include two types of major surgery. They are:
- Oesophagectomy followed by a gastric pull-through and trans-hiatal gastropharyngeal anastamosis
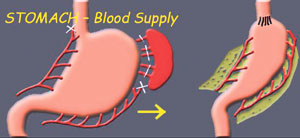
- Oesophagectomy and gastrectomy followed by a colonic pull-through and trans-hiatal colopharyngeal anastamosis and colojejunal anastomosisOesophagectomy followed by a gastric pull-through and trans-hiatal gastropharyngeal anastamosis – under this procedure, all or part of the oesophagus is surgically removed (oesophagectomy) and a portion of the stomach is pulled up into the chest (gastric pull-through) and connected to the remaining portion of the oesophagus (trans-hiatal gastropharyngeal anastamosis). The patient then gets a “new” oesophagus, enabling him to take in food.
Before the surgery, the viability of the stomach is assessed through a laparotomy, explains Dr. Gomez, stressing that only then is the anastamosis (link) of stomach to pharynx decided on.
Thereafter, the neck is opened up, the oesophagus identified and its two ends removed, he says, adding that it is a difficult procedure because it is “blind surgery”. The surgeon cannot see the insides, only feel them with his expert fingers.
One hand has to be inserted on one side and the other from the other side, with the fingers meeting inside the thorax without the surgeon being able to see them, MediScene understands.
The procedure is also not being carried out in an empty space, points out Dr. Gomez. The vital organs such as the heart and the lung are all there along with the major blood vessels. The heart is pumping and the patient could easily go into cardiac arrest.
Once the oesophagus is pulled upwards and surgically removed, a feed tube is attached from the thorax to the stomach which has been temporarily ligated. Then the tube is dragged upwards, bringing the stomach along with it and the stomach fixed to the pharynx.
In some instances, says Dr. Gomez, the surgeon may leave the middle part alone but create an artificial pathway behind the sternum. “This is a blind dissection carried out purely with the fingers,” he says, explaining that there are a few disadvantages, as the passage through the anterior pathway is small due to being surrounded by bone.
This procedure is done, when the surgeon has no other option, MediScene learns, and the patient is advised to take only small meals.
What needs to be taken into consideration when removing the oesophagus is the pyloric sphincter (the ring of muscle which is a one-way valve between the lower end of the stomach and the start of the small intestine) which the surgeon needs to stretch using his fingers or forceps or cut off (pyloroplasty). This helps widen the opening between the stomach and the small intestine.
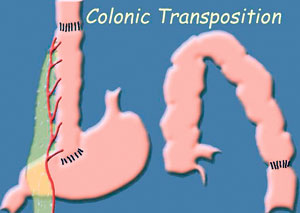
Oesophagectomy and gastrectomy followed by a colonic pull-through and trans-hiatal colopharyngeal anastamosis and colojejunal anastamosis – when the stomach is not viable to be pulled up, then the stomach is also surgically removed (gastrectomy) along with the oesophagus (oesophagectomy). Thereafter the gap in the digestive tract needs to be filled by the large intestine.
Usually, the right side of the large intestine is utilized because of peristalsis (the rhythmic muscular contractions in the small intestine which pushes the food forwards). If the left side of the large intestine where the small intestine is attached to is used, there may be the danger of the food being pushed back to the mouth due to peristalsis. The large intestine is linked to the neck via the previous existing path (after removal of the stomach) or an artificially-created path.
Explaining the anastamosis (links), Dr. Gomez says the horizontal part of the large intestine needs to be made ascending; the upper end of the colon fixed to the pharynx; the lower end of the colon to the jejunum; and the place where the large intestine was linked to the stomach closed.
The anastamoses need to be carried out meticulously, MediScene learns, otherwise leaks can give rise to fistulae and severe infections. Suturing needs much concentration and the correct gaps between sutures maintained. Haphazard suturing will lead to post-operative stenosis.
“Surgeons usually take about 6-9 hours for all these anastamoses but Sir (Dr. Goonetilleke) does it in the record time of six hours,” says the Registrar dwelling on the “artistic manner in which his fingers move”.
|