News
Beware of deadly dengue doing the rounds too

Dr. LakKumar Fernando
Beware the ‘twin’ scourges – COVID-19 and dengue – now doing the rounds in Sri Lanka, cautioned a medical professional on Friday, advising the public on how to respond to this imminent threat.
While COVID-19 and dengue which are viral diseases are affecting people, there are also other viral diseases in the community, said the President of the Association of Medical Specialists (AMS), Dr. LakKumar Fernando who is a Consultant Paediatrician.
He stresses that even if a person gets asymptomatic COVID-19 (disease without symptoms) and is also infected by dengue, the latter can “play up”. Dengue can cause havoc within a person’s system which could lead to Dengue Haemorrhagic Fever (DHF).
Next Dr. Fernando looks at how the two diseases affect different people.
If you are young and healthy, COVID-19 generally hits you as a mild disease. If you are elderly and/or have co-morbidities, COVID-19 hits you badly, causing severe disease and even death.
Dengue is different – whether you are young or old, you can be severely affected by dengue. Another major contrast is that even if you are healthy and well-nourished, dengue can cause severe disease. If in case you have co-morbidities such as diabetes or you are obese, dengue can also cause severe disease.
COVID-19 is largely asymptomatic or mildly symptomatic in children though there may be slightly more severity with the Delta variant. However, dengue causes severe disease in children and could become more deadly than COVID-19. When Sri Lanka had the largest dengue epidemic in recent times in 2017, with close to 200,000 cases and 400 deaths, nearly half of the deaths were of children. But COVID-19 paediatric deaths are a very small percentage.
Dr. Fernando who heads the Centre for Clinical Management of Dengue & Dengue Haemorrhagic Fever in Negombo, says that of 19 ‘fever’ admissions of children to the Negombo Hospital on a single day recently, 15 were positive for COVID-19; 3 for other viral diseases; and 1 for dengue.
His verdict is: There are “lots” of COVID-19 patients, “some” dengue patients and “some” viral fever (other) patients. The danger is that if there is no timely detection and treatment, the dengue patients’ condition can deteriorate.
Dr. Fernando has recently been appointed by the World Health Organization (WHO) to the Regional Technical Advisory Group for Dengue and other arbovirus diseases in the South East Asia Region. His advice to people is:
If a fever (over 100°F or 38°C)lasts more than 24 hours, get a Full Blood Count (FBC), a C-Reactive Protein(CRP) test and a dengue antigen test done between 20-30 hours of the onset of fever.
These tests should not be done too early into the onset of fever. If these tests are done generally at the end of 24 hours of having fever, there are 95% chances of catching an early sign whether the fever is due to dengue.
If there is a history of contact with a COVID-19 positive person or there are respiratory symptoms (sore throat, phlegm, cough and a runny nose), then a Rapid Antigen Test (RAT) or RT-PCR Test should be done to rule out COVID-19.
“A common symptom being manifested by the Delta (Indian) variant is a runny nose, unlike when the wild SARS-CoV-2 first hit Sri Lanka last year or the Alpha (the United Kingdom) variant in more recent time,” says Dr. Fernando.
Another word of advice comes from this clinician on how to protect your family members:
Even if you test negative for COVID-19 or you don’t have symptoms after testing positive, all precautions need to be taken in the next few days to prevent anyone else in your family from contracting this disease. This is due to the virus being in the community.
If you have a fever which is not settling after 3 days, you should undergo either a RAT or an RT-PCR Test.
When asked about numerous pleas from people that they have been abandoned and left to their own devices with no way of getting these basic tests, Dr. Fernando suggests that these desperate people should go to a government hospital if they have tried and failed a private hospital. Government hospitals will do these tests, as they have to ensure that non-COVID-19 patients and wards do not get infected by unwittingly admitting a positive patient.
If anyone is in home-based care (in the ‘Patient Home Isolation and Management System – PHIMS implemented by the Health Ministry), it is important, as suggested by Physicians, to monitor one’s oxygen levels using a pulse oximeter, he says.
Dr. Fernando says that it would be “very significant” if after minimal exertion, there is a drop in the oxygen level. Then the person must go to hospital immediately.
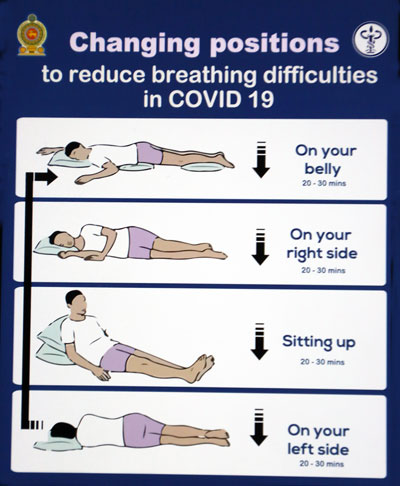
Meanwhile, the Health Promotion Bureau has put out a sketch on how to rest to ensure oxygen preservation to the maximum.