Diabetes is an illness which can affect children as well as adults. Once diagnosed as a diabetic, it is considered as a life-long condition.
Many people do not believe that toddlers and pre-school children can develop diabetes. Yet Diabetes mellitus is one of the most common chronic diseases of childhood. Although the incidence of childhood diabetes is higher in Western Europe and North America, it is prevalent in Asian countries as well.
Is childhood diabetes different from adult diabetes?
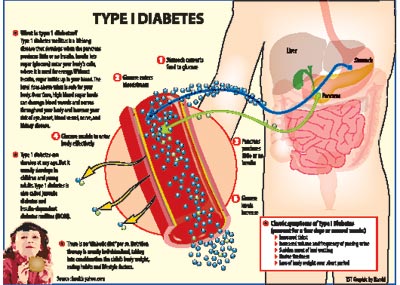
Yes. Diabetes can result either due to reduced secretion of the hormone Insulin from the pancreas or due to defective action of insulin or both. Insulin is the key hormone that controls the glucose level in the blood. In adults who develop high blood sugar or diabetes, the main problem is the defective action of insulin. In children, however, the basic defect is reduced secretion of insulin from the pancreas.
Pancreas is the body organ located in the abdominal cavity and consists of beta cells which secrete the hormone insulin in response to changing blood sugar levels. In childhood diabetes, insulin producing beta cells get self destroyed gradually due to an abnormal immune reaction in the body causing an insulin-deficient state. On the other hand, in adult diabetes there is resistance to the action of existing insulin.
Children with diabetes will need external insulin administration to maintain normal blood sugar levels, whereas adults will need medicines to improve the action of insulin. Adults also might require external insulin in certain situations. Therefore, we call childhood diabetes Insulin Dependent Diabetes Mellitus (IDDM) or Type I Diabetes Mellitus and adult diabetes, Non Insulin Dependent Diabetes Mellitus (NIDDM) or Type II DM.
Type I diabetes occurs in genetically susceptible individuals as a result of progressive, immune-mediated destruction of pancreatic beta cells. Approximately 85% of new cases of type I diabetes occur without an affected parent or a sibling.
The risk to siblings of an affected child is about 6%. The risk to a child of a parent with type I diabetes mellitus depends on whether the mother or the father has type I DM and is 1.3 – 4% or 6-9% respectively. The risk is higher in identical twins. Environmental factors such as viral infections, adverse dietary factors, hygiene and toxins are also found to play an important role in triggering off the onset of the immune process causing beta cell destruction in an individual who is destined to develop immune mediated DM.
Is there a way of predicting that a child is at risk of developing type I DM ?
The risk of developing diabetes both in relatives of a person with diabetes and in the general population can be accurately assessed by special immunological tests. However, as there is no effective preventive intervention, screening is not advised outside the context of experimental work.
Children with newly diagnosed Type I Diabetes usually present with the following classic symptoms for a few days or several weeks.
- Increased thirst.
- Increased volume and frequency
of passing urine
- Sudden onset of bed wetting
- Undue tiredness
- Loss of body weight over short period
Some times children can suddenly go into coma or a semi-conscious state due to very high blood sugar and persistent derangement of the body metabolism.
Type I diabetes presents most frequently during puberty. However, infants, toddlers and preschoolers can also develop Type I DM. A significant proportion of Type II DM also present around puberty due to high prevalence of overweight, obesity and adverse dietary habits among adolescents.
What is the treatment for
Type I Diabetes?
Insulin, diet and exercise are the three cornerstones of Diabetes management. Children with type I diabetes are dependent on life-long insulin therapy. The initial goals of management are metabolic stabilization, providing diabetes education and self-care training for the child (if age and developmentally appropriate) and caregivers (parents, grandparents, older siblings and other care providers).
The diagnosis of diabetes in a child is a crisis for the family and requires considerable emotional support and time of adjustment and healing.
The treatment of childhood diabetes is complicated by factors inherent to childhood. Each phase of childhood has characteristics that complicate treatment, such as unpredictable eating habits of toddlers, unscheduled intense physical play of school-aged children and psycho-social factors that make sugar control a challenging task.
Apart from insulin replacement, dietary management is also a cornerstone of diabetic management. There is no “diabetic diet” per se. Nutrition therapy is usually individualized, taking into consideration the child’s body weight, eating habits and lifestyle factors. There is no evidence that the nutritional needs of children with diabetes differ from those of otherwise normal children. Dietary advice will be provided by the doctor and the nutritionist or the dietician prior to discharge from hospital.
Treatment of a diabetic child is aimed at enabling the child achieve a normal lifestyle with no complications. Complications are seldom seen before puberty even in long standing diabetes. High levels of blood glucose for prolonged periods may cause damage to several body organs like eyes, kidneys and nerves. In fact, diabetic eye disease is a leading cause of blindness among diabetics. All children with Diabetes Mellitus should undergo yearly screening to identify the complications. Early identification enables successful treatment and prevention of further deterioration.
Living with diabetes can be a challenge, but it does not have to stop the child from enjoying life.
(The writer is a consultant
paediatrician and neonatologist) |