Gastro bypasses have hit the headlines in recent times with many views being expressed over this procedure which involves the digestive system.
These bypasses are one type of similar operations which come under “bariatric surgery”, an intervention for people who have “morbid obesity” or severe accumulation of excess weight as fatty tissue, explains a surgeon, stressing that it is not a procedure that should be done for cosmetic reasons.
Morbid obesity is accompanied by serious health problems or co-morbidities that affect almost all organs, says this surgeon who wishes to remain unidentified.The numerous co-morbidities include cardiovascular, respiratory, metabolic, gastrointestinal and psychological diseases.
“Just because you feel that you look fat is not a reason to undergo bariatric surgery,” he says, explaining that even in situations where a person has morbid obesity, bariatric surgery is a last resort, when everything else such as a stringent diet regimen, a strict exercise schedule along with psychotherapy fails.
Before dealing with the different types of bariatric surgery, he explains what morbid obesity is.
A person is considered to be morbidly obese if he/she has a Body Mass Index (BMI) of over 40. The BMI is defined as body weight (in kilograms) divided by the square of the height (in metres), it is learnt
A normal BMI is considered in the range of 18.5-24.9 kg/m2. A BMI of 25-29.9 kg/m2 is considered overweight. A BMI of 30 kg/m2 or greater is classified as obese. He, however, points out that these are standards for the west and should be lesser for Sri Lankans because of their smaller build.
There are many pre-requisites to make a surgeon decide to perform bariatric surgery such as the patient’s life expectancy, MediScene understands. “Usually such surgery is done on young or early middle-age patients,” says this surgeon, adding that other considerations would include whether the patient has at least two other co-morbid factors which could be life-threatening.
“It is very much a case-by-case decision,” he says.
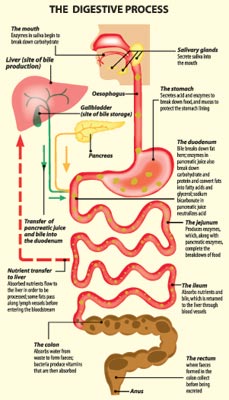
Giving a simple explanation about bariatric surgery, he says that such interventions are carried out to make the patient drastically reduce the quantity of food eaten and to reduce the quantum of nutrients especially fats, absorbed by the body (malabsorption). It makes the stomach smaller and allows the food to bypass part of the small intestine or bowel-- comprising the duodenum, jejunum and ileum -- where most of the nutrients and calories are absorbed to the body. (See sketch of how food is digested) “This leads to weight loss,” he says.
There are two ways through which bariatirc surgery can be carried out – by opening up the abdomen or by making a small incision and inserting a laparoscope, MediScene learns.
The three basic concepts for bariatric surgery are:
- Gastric bypass or restriction through adjustable gastric banding or sleeve gastrectomy – only reducing the size of the stomach. This is a “restrictive surgical procedure”. Adjustable gastric banding involves fitting a band around the stomach, which can be adjusted by the surgeon, making it tighter or looser depending on the amount of food that should be taken by the patient. A gastrectomy is the surgical removal of all or part of the stomach.
- Gastric bypass or restriction with mild malabsorption through a Roux-en-Y gastric bypass – reducing the size of the stomach as well as reducing the length of the small intestine to a lesser degree. This is a “restrictive procedure with some malabsorption”.
- A combination of mild gastric bypass or restriction and malabsorption through a pancreatic diversion with duodenal switch – reducing the size of the stomach to a lesser degree as well as reducing the length of the small intestine to a larger degree. This is a “malabsorptive procedure with some restriction”.
Gastric bypass
Under this procedure, a small thumb-sized pouch is created from the upper stomach (which can retain only 15–30 ml or 1–2 tbsp), accompanied by a bypass of the remaining stomach. This restricts the volume of food which can be eaten. The stomach may simply be partitioned by the use of a plastic band or surgical staples or may be totally divided into two parts also with staples.
Roux-en-Y gastric bypass (proximal)
In a Roux-en-Y gastric bypass, the stomach is made smaller by creating a small pouch at the top of the stomach using surgical staples or a plastic band as mentioned earlier. Then the smaller stomach is connected directly to the middle portion of the small intestine (jejunum), bypassing the rest of the stomach and the upper portion of the small intestine (duodenum).
The small bowel is divided about 45 cm (18 in) below the lower stomach outlet, and is re-arranged into a Y-configuration, to enable outflow of food from the small upper stomach pouch, via a “Roux limb”.
In the proximal version, the Y-intersection is formed near the upper (proximal) end of the small bowel. The Roux limb is constructed with a length of 80 to 150 cm (30 to 60 inches), preserving most of the small bowel for absorption of nutrients. The patient experiences very rapid onset of a sense of stomach-fullness, followed by a feeling of growing satiety or “indifference” to food, shortly after the start of a meal.
Roux en-Y gastric bypass (distal)
The normal small bowel is 600 to 1000 cm (20 to 33 feet) in length. As the Y-connection is moved farther down the gastrointestinal tract, the amount of bowel capable of fully absorbing nutrients is progressively reduced. The Y-connection is formed closer to the lower (distal) end of the small bowel, usually 100 to 150 cm (40 to 60 inches) from the lower end of the bowel, causing reduced absorption (malabsorption) of food, primarily of fats and starches, but also of various minerals and fat-soluble vitamins. The unabsorbed fats and starches pass into the large intestine, where bacterial actions may produce irritants and malodorous gases.
Biliopancreatic diversion with duodenal switch
Under this procedure, a gastrectomy is performed resulting in a tubular stomach. Then the duodenum is divided past the pyloric valve and the ileum is also divided. The distal or lower end of the small intestine is anastomosed (joined) to the proximal duodenum (first section of the small intestine) and a common channel created distally with Y-anastomosis. |