A bouncy baby boy is in the home and the new parents have their hands full. Each day it is a joyful experience. But be watchful -- for one in every 200 baby boys may have a problem which is easily correctible if detected early.
If parents notice their baby son passing urine in a strange manner, they should consult a paediatric surgeon, a uro-genital surgeon or a reconstructive surgeon, MediScene understands.
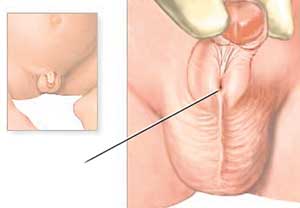
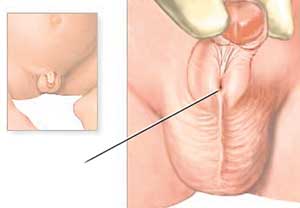
If the baby boy's urine sprays around and there is no direct stream then he may be having a condition called hypospadiasis, says Reconstructive Surgeon Dr. Lalantha Amarasinghe, explaining that it is the displacement of the urethral opening (meatus).
 |
| Urethral Opening |
The urethra is the canal through which both the urine and the semen are discharged in males. While the urethra carries urine from the bladder and discharges it through an opening at the end of the penis, this canal is also connected to the prostate gland and seminal vesicles and testes and transports semen received from those organs.
In hypospadiasis also known as hypospadias, which is present from birth, the urethral opening is abnormally placed, MediScene understands. "Without opening at the tip of the glans (rounded head) of the penis, as is normal, the urethra may open anywhere along a line from the tip along the underside of the penis to the junction of the penis and scrotum or perineum," says Dr. Amarasinghe.
Considered to be one of the most common birth defects in the genitalia (sex organ) of boys, he says that it occurs while the baby is still in the mother's womb. It is due to the pituitary gland failing to secrete certain hormones such as prolactin and also testosterone secretion anomalies during foetal growth. No strong hereditary link has been established, he says. About 7-10% of cases may be familial (hereditary).
Regrettably, hypospadiasis is not spotted in many cases during the initial medical examination of the baby at birth, he adds.
Dr. Amarasinghe categorizes hypospadiasis, depending on where the urethral opening is.
- Glanular hypospadiasis occurs when the urethral opening is just below the end of the penis.
- Coronal hypospadiasis is when the urethra opens in the groove where the head of the penis meets the shaft.
- Distal penile hypospadiasis is when the opening is anywhere along the underside of the shaft of the penis.
- Perineal hypospadiasis occurs when the urethra opens in the scrotum and is the most severe type of hypospadiasis where the testes tend to be pushed aside.
A common problem for boys who have hypospadiasis, explains Dr. Amarasinghe, is difficulty in passing urine, while standing, with the stream of urine splattering all over. "Then boys have to sit like girls when passing urine and it is imperative that hypospadiasis is corrected before they go to school at five years of age.
Otherwise they will be bullied and laughed at by their classmates," he says.
The cosmetic appearance of the penis is also different from other boys and can lead to anxiety in the little one, according to Dr. Amarasinghe and if not corrected, in adulthood may be associated with infertility.
Dealing with a condition called chordee where the head of the penis curves downward, due to coronal hypospadiasis, he says that the curvature occurs due to part of the urethra developing a fibrous band.
Stressing the need for surgical correction as early as possible, he says that it is a simple but skilful operation. "The surgeon has to be dexterous at fine darning," smiles Dr. Amarasinghe adding that in this technique, a urethral opening is created on the tip of the penis and the foreskin is used for surgical reconstruction.
Performed under general anaesthesia, the surgical correction of hypospadiasis would follow a few steps depending on its severity.
If there is no chordee, we do an erection test and a one-stage repair - Snodgrass repair -- by making a groove or drain on the underside of the penis leading to the head of the penis and covering the whole thing with foreskin.
If there is chordee then it is a two-stage repair, called the Aivar Bracka Repair with the fibrous band having to be removed first and the glan being split before the opening is brought to the tip of the penis. The first stage of surgery would be performed when the boy is about 3 ½ years old and the second stage at 4 ½ years old, with a seven-day stay in hospital each time because a catheter has to be fixed for the urine, says Dr. Amarasinghe. "After these repairs, which take about two hours each, the penis takes on a normal appearance and the child can go to school at five years of age without any fear or concern."
What of the risks
of surgery?
Hardly any, assures Dr. Amarasinghe, if the surgeon is skilled. The two most common and easily overcome problems are the formation of a fistula through which there could be leakage of urine along the suture line or a urine infection.
The fistula can be repaired and the infection can be treated with medication.
Importance of foreskin
An integral part of the repair of hypospadiasis is the foreskin. Do not circumcise your child for religious or other reasons without examination by a doctor, says Dr. Amarasinghe.
If the foreskin is removed during circumcision and your child is diagnosed with hypospadiasis after that, the foreskin required for grafting would not be available to the surgeon, he says adding that then the only option would be to take mucosa skin from the inside of the child's mouth, increasing the morbidity of surgery.
|