News
‘No community transmission but need a behavioural change among people’
There are two active COVID-19 clusters but no community transmission of this viral disease, assured a high level health official on Thursday evening.
Pointing out that currently the navy cluster and the Kuwaiti-returnee cluster are the only two active ones pushing up the number of patients, the Health Ministry’s Chief Epidemiologist Dr. Sudath Samaraweera in a wide-ranging interview with the Sunday Times explained that the cases from the community the country had were limited to ‘family clusters’.

Dr. Sudath Samaraweera
The reported number of ‘confirmed’ positive cases of COVID-19 showed:
· The cluster of navy personnel and their close contacts as of Thursday were 727, with 53 including the navy driver from the Gaffoor Building in Fort being on May 27.
· The West Asia returnee cluster stood at 430 on Thursday.
The last ‘family cluster’ at Dabare Mawatha in Narahenpita ended on April 30. These ‘family clusters’ come about when a person infects relatives, friends or neighbours within a certain area. However, in ‘family clusters’ we know how it started, unlike in community transmission where there is no indication from whom people in the community have got infected, said Dr. Samaraweera.
“When community transmission comes that means there will be cases coming up here and there with no link among these cases,” he said.
While many experts commended Sri Lanka at the way it has handled the epidemic, they also expressed certain concerns. These include – why the navy cluster is still active and has not been contained; how Sri Lanka should face the challenges posed by infected returnees; whether the strain infecting returnees is more virulent than the one already in Sri Lanka; whether hospitals treating COVID-19 would be able to manage such a large number of infected returnees; and whether the newly-opened hospitals for the management of these patients have the requisite facilities?
Focusing on the navy cluster, Dr. Samaraweera said the first case was reported on April 22, but that did not mean that he would have been the first to get infected. Even in his case he would have got it maybe one week before.
 He said: “We think that the virus might have been circulating within the very large 300-acre Welisara compound, which is like a city, and home to many units comprising around 5,000 personnel living in close proximity, for quite some time, maybe even several weeks.
He said: “We think that the virus might have been circulating within the very large 300-acre Welisara compound, which is like a city, and home to many units comprising around 5,000 personnel living in close proximity, for quite some time, maybe even several weeks.
“When we detected the trigger (the first reported case) and began control activities, there could have been some patients who had already got the disease and had been cured (asymptomatic). Some people may be at the late stage of the disease now and some maybe in-between. There is a spectrum of cases.
“The spread of the virus is in one or two units while others have not been affected. We have segregated them and they are at different places. It will take another couple of weeks to reduce that number. Usually a cluster can be brought under control within two incubation periods (28 days). Now a month has passed and it is still ongoing. Once the level of cases has been lowered, then it will take two more incubation periods for it to be completely sorted out.”
With regard to testing, Dr. Samaraweera said that the returnees from abroad were not being tested at the airport but sent to quarantine centres and if symptoms manifest the tests are done. This is while there is random testing of high-risk groups such as bus drivers and conductors, trishaw-drivers, vendors at marketplaces, etc. Since Sri Lanka does not have community transmission, there is no requirement for blanket testing.
Referring to the chance of returnees bringing back a more virulent strain of the virus, he said that there is no such thing as virulent and non-virulent strains. There are three clades (types) and some sub-types. No sequencing has been done yet to identify the clade which has infected the returnees.
“We will keep bringing back these people from West Asia on humanitarian grounds. Many of them have been given an amnesty to leave Kuwait and we are ethically and dutifully bound to bring them back. But it will not be fast tracked as we need quarantine facilities, laboratory capacity to test them as well as the ability for our health system to handle larger numbers. We should also prevent opportunistic leaks from happening such as the virus getting into the community through the drivers or others who come into contact with them,” he said.
Referring to the relaxation of the lockdown and the curfew, he said that in certain instances crucial measures such as social distancing and face-mask wearing were not happening with the incident in Maligawatte where three women were trampled to death in a crowd of around 500 was ample evidence of this. Even when people are boarding buses this can be seen.
Asked whether this is because the right message has not gone to the people, he said people had knowledge about these measures but what was needed was a behavioural change for which they were not geared.
Looking at the issue of whether the new hospitals being opened for the management of COVID-19 had the required facilities, Dr. Samaraweera said that it is the asymptomatic people who would be sent to these hospitals such as Teldeniya, Hambantota and Kattankuddy. They do not need treatment, only monitoring, simple medications such as paracetamol, nutrition and comfort. If they develop symptoms they will be transferred to a hospital with good ICU facilities.
When asked about the 10th death, Dr. Samaraweera said that it may not have been a direct COVID-19 death. Her death was due to a myocardial infarction (heart attack) and she tested positive only after she died.
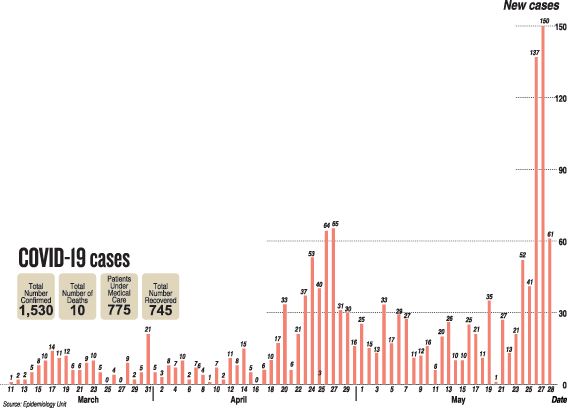
| The waves and peaks of COVID | |
| Waves and peaks – this is what former Chief Epidemiologist Dr. Nihal Abeysinghe explains with regard to the COVID-19 outbreak. Sri Lanka is still having the first wave of COVID-19, which in turn has several peaks. Dr. Abeysinghe gives the figures before flagging the peak of the first wave: up to March 13 – 5 cases; March 14th to 20th – 66 cases; March 21st to 27th – 34 cases; March 28th to April 3rd – 53 cases; April 4th to 10th – 38 cases; April 11th to 17th – 47 cases; April 18th to 24th – 176 cases; April 25th to May 1st – 271 cases; May 2nd to 8th – 145 cases; May 9th to 15th – 100 cases; May 16th to 22nd – 133 cases; and May 23rd onwards – 300 plus cases and rising. As such the first peak occurred between April 25th and May 1st (271 cases) while the second peak may be this week or much later, he says. Harking back to the Spanish flu which hit the world in 1918, he says there had been six waves. This can go on until a vaccination is developed and people get their shots. The government, meanwhile, has to take a policy decision whether we are going to keep all these positive cases at home or in hospitals. So far they have been in hospitals but now we need to think whether it is worth keeping them hospitalised as there is a two-way risk, said Dr. Abeysinghe. He added that one is that if these patients don’t have symptoms, it is taken lightly. The other is that if hospitals get filled up, they would not be able to handle it. |
Don’t panic – there is no increase in Kawasaki Disease after COVID-19

Prof. Pujitha Wickramasinghe
Don’t panic. There is no increase in Kawasaki Disease among children in Sri Lanka after the COVID-19 outbreak.
This was the strong reassurance given to parents by well-known Paediatrician, Prof. Pujitha Wickramasinghe, following speculation and fear that Kawasaki Disease is on the rise in the country.
Earlier, international reports from the United Kingdom, the United States of America, Spain, France and Italy referred to a possible “new phenomenon” describing it as being similar to Kawasaki Disease and Toxic Shock Syndrome.
Pointing out that Kawasaki Disease is not new to the world having been identified in 1967, Prof. Wickramasinghe who is Senior Professor in Paediatrics at the Faculty of Medicine, University of Colombo, and Honorary Consultant at the premier Lady Ridgeway Hospital (LRH) for Children, says that no one knows exactly how the illness starts.
The cause of Kawasaki Disease is not known but it leads to the inflammation of blood vessels. It is not infectious and does not spread from child to child. It is diagnosed on clinical signs and symptoms and it is treatable, he said.
The signs and symptoms associated with Kawasaki Disease are fever going on for five days or more, itchy red eyes but without the production of pus, cracked lips and red mouth but there is no ulcer formation and enlarged lymph nodes in the neck, the Sunday Times learns.
“If your child is having fever, give him/her paracetamol, lots of liquids and whatever he/she wishes to eat. Watch for 48-72 hours and if the fever does not subside, see a doctor,” says Prof. Wickramasinghe, explaining that no diagnosis can be made in one or two days.
Referring to the prevalence of Kawasaki Disease, he says that though the numbers across the country are not known, at LRH they see about 10-15 cases per year.
“There is treatment for Kawasaki Disease, so don’t panic. It is only rarely that complications such as the heart’s blood vessels being affected arise,” he adds.
| A message to parents | |
|
Good antibody testing a need as country moves into next phase

Dr. Mahen Kothalawala
Sri Lanka has fared well in tackling the COVID-19 epidemic but it is time for a review to continue the positive measures and change the negative measures, urges Kandy National Hospital’s Consultant Clinical Microbiologist, Dr. Mahen Kothalawala.
A point brought into focus is how the testing protocol is linked to COVID-19 outbreak control, with emphasis on the need to move into quality antibody testing to get a feel of what is happening in the community.
In the early phase, many measures such as the lockdown and curfew were imposed along with intensive RT-PCR (Reverse Transcription-Polymerase Chain Reaction) testing to separate the infected from the non-infected and contact tracing was carried out.
Getting into technicalities, Dr. Kothalawala says that in a real time PCR assay a positive reaction is detected by the accumulation of a fluorescent signal. The Ct (cycle threshold) is defined as the number of cycles required for the fluorescent signal to cross the threshold. Ct values are inverse to the amount of viral nucleic acid which is in the sample. A low Ct valueindicates a high viral load and a high Ct value means a low viral load.
It’s usually in symptomatic patients that the viral load would be high giving a low Ct value. This would be different to those who are mildly symptomatic or asymptomatic, he says.
So the ‘containment’ protocol followed by Sri Lanka is to hospitalize, isolate and treat the infected persons, while netting in their contacts through tracing; placing them in quarantine for 14 days and conducting RT-PCR tests on Day 7 and Day 14. If the two tests are negative, they are sent home. If they become positive they are hospitalized.
This was to ensure that there are no chances of infected people giving the disease to others, says Dr. Kothalawala, pointing out that when people are quarantined for 14 days the chance of missing someone who is infected is 1 in 10,000. This is while in countries which quarantine people for only seven days, the chance of missing them would be 21 in 10,000.
He reiterates that this was all in the First Phase and now Sri Lanka is in the Second Phase of living with COVID-19. There is the possibility that despite all efforts to remove positive patients from the mainstream through RT-PCR testing and contact tracing, some pre-symptomatic, mildly symptomatic or asymptomatic people fall through this testing net.
How this can occur is:
· There is a ‘window’ when conducting RT-PCR testing if the viral threshold is low (the RNA is inadequate), when there could be no definitive confirmation. This could occur two days before symptoms manifest or three days after mild symptoms manifest.
· The other possibilities are when a good sample is not secured by a trained person or if the person from whom the sample is being taken is uncooperative.
· The RT-PCR machine too should be optimized to meet the sensitivity of different reagents that may be used.
There is a 71-98% variation in getting the right result with a conservative estimate being 70%, he says.
This is why, Dr. Kothalawala is recommending that as Sri Lanka steps into Phase II, it should seriously think of establishing good antibody testing among the population.
“Antibody testing should not be to identify the acutely infected people but to check the spread and find out how many people have got an exposure to the virus,” he says.
Looking at the different types of antibody tests, he says that the rapid antibody test and the rapid antigen test also called the cartridge test have low sensitivity of around 40%. The ELISA test (an enzyme-linked immunosorbent assay) and the chemiluminescent test (CLT), however, are highly sensitive.
He points out that the ELISA reader is widely found in universities, hospitals as well as the Medical Research Institute (MRI) and the need is to buy reagents under certification from the National Medicines Regulatory Authority (NMRA). Some ELISA tests have 99% sensitivity and 100% specificity.
Many countries such as Israel, China, America, France and the United Kingdom are using antibody testing as a supplementary exposure test in addition to the diagnostic RT-PCR test.
Dr. Kothalawala also refers to a 45-minute RT-PCR cartridge based nucleic acid amplification test, different to the RT-PCR test which takes 6 hours and says the first one could be used at the airport as a point-of-care test for high-risk people coming through.
“We have these machines with a tuberculosis platform in every district which can also be used as an on-demand test rather than the batch test being performed now,” he says, adding that incorporating these aspects would help smoothen out the containment phase.
| Immunity Passports | |
| If we conduct proper mass-scale antibody testing, we can issue ‘Immunity Passports’ to those who show antibodies and make use of these people as volunteers to help in the battle against COVID-19, says Dr. Mahen Kothalawala, stressing that the World Health Organization (WHO) has stated that people who have been exposed to the virus would not be re-infected.We don’t know how long this immunity would last, whether it is lifelong or short-term, but we do know that it would be for at least six months, he say |
Anti-malaria drug off the table in COVID treatment
Hydroxychloroquine, which was being touted as the “wonder” medicine in the treatment of COVID-19 may be turning out to be a damp squib, with the World Health Organization (WHO) temporarily suspending experiments with this anti-malarial drug.
The suspension followed safety concerns highlighted in a study titled ‘Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis’ published in the medical journal ‘Lancet’ on May 22. It had indicated a higher mortality rate and heart problems among patients receiving the drug alone or with a macrolide.
Hydroxychloroquine was one of four treatment options that were being compared against the standard of care in the WHO’s Solidarity trial. Nearly 3,500 patients from 17 countries have already been enrolled in the study.
The other three arms of the Solidarity trial are: Remdesivir (an antiviral drug used against Ebola); Lopinavir with Ritonavir (a combination in the treatment of HIV/AIDS); and Lopinavir with Ritonavir plus Interferon beta-1a (a mix used in the treatment of HIV/AIDS and multiple sclerosis).
| Timeline | |
| May 21- 27 cases were reported, 11 of them navy personnel, 15 returnees from Dubai and 1 returnee from Kuwait.May 22 – 13 cases were reported, 11 of them navy personnel, 1 returnee from Malaysia and 1 returnee from Kuwait. May 23 – 21 cases were reported, 19 of them navy personnel and 2 returnees from Dubai. May 24 – 52 cases were reported, 49 of them returnees from Kuwait, 1 returnee from Indonesia and 1 from the navy. May 25 – 41 cases were reported, 40 of them returnees from Kuwait and 1 returnee from Dubai. Meanwhile, a 51-year-old woman who had returned from Kuwait and was in quarantine in Trincomalee died, pushing the death toll from COVID-19 to 10. She had been a heart patient. May 26 – 135 cases were reported, 127 of them returnees from Kuwait and 8 navy personnel. May 27 – 150 cases reported, 97 of them returnees and 53 navy personnel. This was the highest number of patients reported in a single day in the country since the first local was diagnosed with the new coronavirus on March 10. May 28 – 61 cases were reported, 35 of them returnees and 26 navy personnel.
|


