News
Will it be DF or DHF – answer from our antibody response to the NS1 toxin
Tropical countries including Sri Lanka have been battered and bruised by dengue for a long time in recent memory. The tiny mosquito with white-striped legs has gone into homes and schools, spreading death and disease through this viral disease.

Scientist Deshni Jayathilaka with other team members in the background in the laboratory of the Centre for Dengue Research. Pic by Amila Gamage
Dengue has turned into the plague of recent times coming in all its fury as the rains patter down, leaving parents in a stranglehold of fear. Dengue epidemics have flooded hospitals across the country with men, women and children over the years.
Many discussions, meanwhile, have had as their focus the NS1 antigen test linked to the early detection of dengue.
No one, though, had looked at the NS1 or non-structural protein 1 of the dengue virus and the antibodies created in response to it in humans.
But a pioneering team of scientists from the Centre for Dengue Research — headed by Prof. Neelika Malavige – of the Sri Jayewardenepura University has done just that. They have come up with landmark findings, unveiling the secret which will answer the crucial question – who will get mild dengue (Dengue Fever – DF) or severe dengue (Dengue Haemorrhagic Fever – DHF).
The team’s findings are a first in the world and have been published in ‘Nature Communications’, a peer-reviewed, high-impact scientific journal, last month (December 2018).
These experiments which will have a major impact on the treatment and management of dengue in the future were the work of a doctoral student Deshni Jayathilaka and Senior Scientific Researcher Laksiri Gomes. The other members of the team were Dr. Chandima Jeewandara, Dr. Danushka Herath, Dr. Samitha Fernando, Dr. Geethal Jayaratne and Dr. Pathum Perera. The external collaborators were Dr. Ananda Wijewickrama from the National Institute of Infectious Diseases, Angoda and Prof. Graham Ogg and Dr. Clare Hardman from the University of Oxford, United Kingdom.

Prof. Neelika Malavige
Explaining that the NS1 antigen (a toxin), when it enters our bodies causes the creation of antibodies (due to the immune response in the body), Prof. Malavige says that no scientist had looked at these antibodies in humans closely. There have been studies in mice with varying results but no such studies of the impact of the NS1 antigen antibodies in humans before.
“The dengue virus does not cause disease in other animals, only humans are adversely affected,” says Prof. Malavige on Monday, seated in the state-of-the-art laboratory of the Centre for Dengue Research, while three of her team members are peering into microscopes or sorting out test-tubes.
Isn’t it obvious that we need to study the antibody response to the NS1 antigen in humans themselves, she laughs..……and this is what her team did.
Looking at the dengue virus, Prof. Malavige says that there are four strains or serotypes – DENV1, DENV2, DENV3 and DENV4. All these serotypes have the NS1 protein which is unique to that particular serotype.
The team studied how the NS1 protein antigen and the antibodies created as a response to it in humans behave. Was the behaviour good or bad for the human?
But it was not that simple – for to study the antibodies created in response to the NS1 antigen, there was a need to measure them.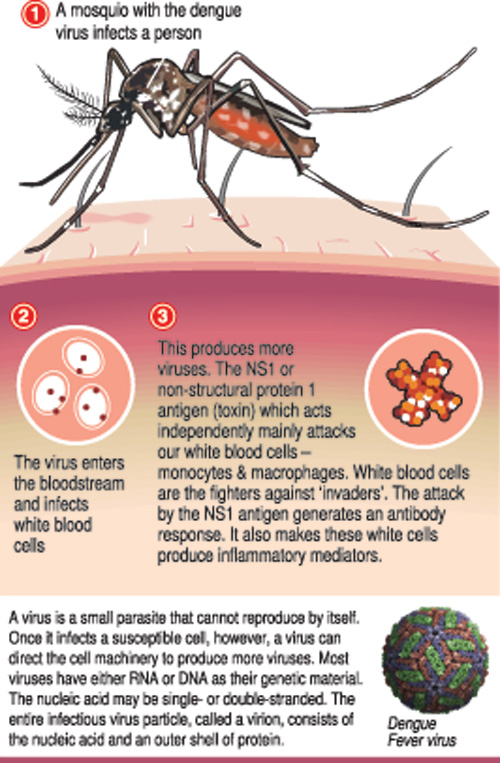
This measurement is called an assay, she explains, and there was no commercial assay anywhere in the world. Undaunted, her team set about developing this assay. That was about 2½ years ago.
“It took about nine months to develop the assay and then fine-tune (optimize) it, as we had to do everything from scratch,” says Prof. Malavige.
It was not one but two assays that they developed – to look at antibodies created by the human body to the whole of the NS1 protein and to check the antibody response against the different regions of the NS1 protein. (See box for landmark findings)
The hard work has been fully worth it – the research they have conducted very successfully, but for them the most fulfilling part is that in the future it would help patients.
| Study will pave way to develop biomarkers and a good vaccine | |
| The NS1 antigen (toxin) is a “nasty” piece of work, reiterates Prof. Neelika Malavige, explaining its ‘profile’ before focusing on her research team’s findings. When the mosquito carrying the dengue virus takes a bite and injects this virus into the human body, the NS1 antigen acts as a separate entity within the body. It secretes protein which causes a lot of trouble – attacking the white blood cells called monocytes and macrophages both vital in fighting off ‘invaders’ like viruses and also many other cells. When attacking the monocytes and macrophages, the NS1 antigen makes these cells in some people to produce inflammatory mediators causing severe disease. Prof. Malavige and her team have discovered that the type of antibodies created due to the invasion of the NS1 antigen differed in those with mild disease (Dengue Fever — DF) as opposed to those who were struck by severe disease (Dengue Haemorrhagic Fever — DHF). The results are likely to pave the way to further understand why only some people develop very severe disease but others have mild or asymptomatic (showing no symptoms) illness. Spectacular findings which will help in the development of a biomarker (in medicine, a biomarker is a measurable indicator of the severity or presence of some disease state) for dengue as well as a good vaccine which has protective antibodies against NS1. Prof. Malavige says that in the case of a biomarker, it would be helpful in differentiating between mild and severe illness which, in turn, would lead to fewer people having to undergo close monitoring in hospitals at the cost of much time, effort and money. “Then we will be able to pick out those who have DF and DHF, with admission to hospital being required only for those with DHF.” Referring to the development of a vaccine against dengue, she stressed that the antibodies which are created to the NS1 antigen in severe dengue would be very useful. However, there is a lot more work to be done to fully understand how different types of NS1 antibodies are generated and the mechanisms through which they cause severe dengue. So far, one dengue vaccine — Dengvaxia® (CYD-TDV) — developed by Sanofi Pasteur has been licensed in some countries, while five more dengue vaccine candidates are in clinical development or in the pipeline. Some experts across the world speculate that the “less than expected efficacy” of Dengvaxia may be due to the lack of the generation of antibodies against the NS1 antigen. |

