Sandun will talk again, eat again
Sadun Chathuranga Wijekoon sports a colourful neck-scarf when we meet him in late July.
It is not an accessory to make this 23-year-old from Wewagama about 12km from Kuliyapitiya dapper but to hide a plaster, which is covering sutures which are scheduled to be removed the day we meet him just outside the Ear-Nose-Throat (ENT) Clinic of the National Hospital of Sri Lanka (NHSL).

Sandun after the procedure (above) and (inset ) with the tracheostomy tube
That day, he is all smiles – for a young man who had earlier been told he would have a tracheostomy tube all his life and would only be able to speak with a hoarse voice, with the words being unclear, all those medical predictions have been proven wrong.
After many other failed attempts, a first in Sri Lanka has worked for him.
The ‘first’ is the removal of a supraglottic haemangioma through Coblation Technology performed on Sandun by trailblazing ENT Surgeon Dr. Rizny Sakkaff who is also a very skilled Head and Neck Surgeon, with many other firsts to his name.
In Sadun’s case, a slight slip or a minute error would have cost him dearly. A supraglottic haemangioma is a collection or cluster of small blood vessels that form a lump just under the mucosa in the upper part of the larynx (voice box), including the epiglottis, the area above the vocal cords, MediScene learns.
Before going into detail about the procedure, through which Dr. Rizny ventured into an area where no one had dared to go, he says that the haemangioma blocking the airway was so big that Sandun’s vocal cords could not be seen.
“Everything was blocked,” says Dr. Rizny, pointing out that Sandun could not breathe nor talk properly.
No doctor was ready to touch the haemangioma, which was interior to the Adam’s apple, for they were worried about the complications of this congenital malformation of blood vessels. The repercussions could be disastrous – massive bleeding which could easily lead to death, MediScene learns.

Dr. Rizny Sakkaff
Various treatments had been attempted, including measures to shrink the veins by injecting a sclerosing solution and laser surgery when an Indian expert tried it out on Sadun, but to no avail. Finally, Sandun had been told that he would have to “live with it”.
Sandun’s medical saga had begun on a December day in 2012 when paan kellak kala ugere hiravuna, he says, explaining that he had choked on a piece of bread. He was in his OL year.
With large gulps of water he was able to swallow the piece of bread but there was much vomiting stained with blood. His terrified family rushed him to the Kuliyapitiya Hospital, where they “camera demma” (did an endoscopy) and then transferred him to the NHSL. That evening itself, as he was finding it difficult to breathe, a tracheostomy tube had been inserted. [A tracheostomy tube is inserted into a tracheostomy stoma (a hole made in the neck and windpipe (trachea), bypassing the mouth, nose and throat.]
Three days later, as he was finding it difficult to swallow, another tube had been inserted – nasogastric intubation (NG tube) — through the nose, past the throat and down into the stomach to feed him. A month later, urged to take soft foods, the NG tube had been removed.
A young life was in disarray – he could not sit the OL examination, he couldn’t speak and he couldn’t eat properly. With his studies being disrupted, he joined a garment factory close to his home to stitch T-shirts. Falling in love with co-worker, Ruwanthi Lakmali, Sadun was facing a dilemma whether he should marry her as he was a sick man.
Many were the visits to hospital, when he was told by the NHSL staff to go to the Kuliyapitiya Hospital as it was closer home. On April 4, he met Dr. Rizny there but soon after Dr. Rizny had been transferred to the NHSL. When Sadun got a pain in his throat again, he came back to the NHSL.
He believes that it is destiny, for it was when his paths crossed that of Dr. Rizny that there was hope of a permanent cure for this hapless young man.
When we meet Sadun that day, there is laughter and joking among him and the ENT staff. Sadun and his sweetheart had been married on Vesak poya, April 28, before Dr. Rizny performed Coblation Technology on him. There had been implicit faith that Sadun would get back his voice, rid himself of the tracheostomy tube and also be able to enjoy the food that his wife cooked for him.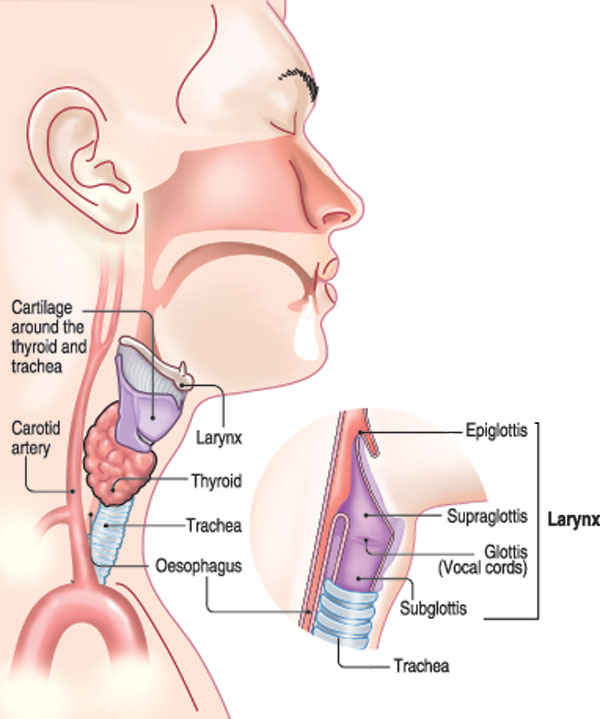
| The procedure that requires great skill Coblation Technology, a minimally-invasive procedure, though used in other parts of the body to deal with haemangiomas has never been tried in ENT surgery in Sri Lanka, says Dr. Rizny Sakkaff, before explaining what it is all about.‘Coblation’ is ‘controlled ablation’ and Coblation Technology is a controlled, minimal-heat driven process. It uses radiofrequency energy to excite electrolytes in a saline (sodium chloride – NaCl) solution, creating energized ionized particles in plasma, explains Dr. Rizny, pointing out that the ions then bombard tissue in their pathway, making the tissue to dissolve.It occurs at very low temperature because the heat generated is used up by the ionization process. As such, minimal damage is caused by the heat to the tissue on the periphery of the haemangioma, he says. Referring to this special technology, delivered after the patient is placed under general anaesthesia, Dr. Rizny says that the energy is provided through a hand-held instrument which is placed in the mouth. Immense skill is needed for absolute caution on the part of the surgeon, MediScene understands, with a slip or error leaving behind a trail of harm. The tracheostomy tube had been kept in place with a cap for a few days to make sure that he could breathe normally and then removed, with sutures to hold together the incision made earlier to insert the tube. The day we meet Sandun, the sutures are removed and the plaster is discarded. Usually, there would be a nasty ragged scar where the tube had been taken off – but in Sadun’s case it had healed well, leaving no ugly mark. For Sandun and Ruwanthi, an unforgettable wedding present from the gifted hands of Dr. Rizny – the haemangioma no more, breathing sans the tube, a normal voice and the ability to eat without constriction. | |


