Getting a life after chronic liver disease
The first-ever transplant in Sri Lanka for acute liver failure was performed by the Colombo North (Ragama) Hepatobiliary and Liver Transplant Unit on July 20.

The team which performed the first transplant for acute liver failure on July 20 caught on camera after the operation
What many may not realize, however, is that it is just one more feather in the cap of this unit par excellence which has taken liver transplantation to a different level, making it a fine art to benefit people, who otherwise would have to seek treatment abroad.
The numbers speak for themselves – the unit has been saving from the jaws of death those suffering from chronic liver disease for which the only answer is a transplant, not only with livers from brain-dead people (cadavers) but also from living donors.
Since the unit was established in February 2012, it has performed transplants with 13 deceased-donor livers and five from living-donor liver sections, with a success rate of 70%. The first transplant with a liver from a deceased donor had been earlier, in May 2011.
MediScene learns that the number of patients referred for transplant assessment is 120 per year and the number of patients listed (having completed work up and ready for deceased donor transplant when a liver is available) is 4 to 5 patients from each blood group at any given time. However, not all patients are eligible for transplant as in some cases they are unsuitable while sometimes limited resources also hinder the unit’s work.

Hemamali on a routine visit to the clinic with husband Peiris. Pix by Priyantha Wickramaarachchi

Dr. Madunil Niriella
Exactly five months after she got a brand new liver from a brain-dead donor, 59-year-old Hemamali Amarasekara, accompanied by her husband, C.L.W. Peiris, both retired teachers, is at the Colombo North Hepatobiliary and Liver Transplant Clinic for a routine check-up on August 9.
When MediScene pays a visit to the clinic they are among other patients awaiting their turn to see the panel of doctors. With two grown-up children, life was normal, until six and a half years ago Hemamali began vomiting blood one night. She had experienced a loss of appetite over time, but only realized that something was wrong when the next day a shock awaited her when she used the toilet. The commode was full of blood.
The hospital visits and loads of tests followed, with advice that she consults a “good” Physician, as there seemed to be no cure in this country for this illness. “Ende, ende kettu wuna,” recalls her husband, explaining how they came across another patient who was seeking treatment for a similar ailment at a private hospital in Colombo. They did the same and blood reports as well as an endoscopy were ordered. During the endoscopy, Hemamali’s stomach was banded to stop the bleeding.

Dr. Rohan Siriwardena
Her gall-bladder too was swollen and stones were removed from that while it was also diagnosed that she was suffering from non-alcoholic cirrhosis. What the family saw was that Hemamali was wasting away………..davasin, davasa diranna patan gaththa, apita balagena inna beriwuna, says her husband and the desperate family started the search for the “best” place to seek treatment, talking to people and surfing the net.
Coming across the one-and-only Hepatobiliary and Liver Transplant Unit functional in the country at the Colombo North Teaching Hospital, it was here that the family which was mentally devastated got some confidence that they could even think of making Hemamali well again.
“Bayawenna epa (don’t be frightened),” assured Consultant Gastroenterologist and Hepatologist, Dr. Madunil Niriella, explaining that what Hemamali required was a liver transplant.
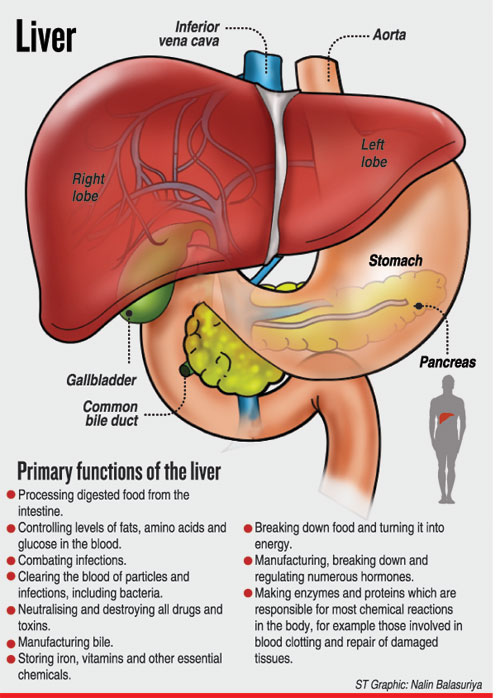
Before delving into the details of a transplant, Dr. Niriella talks of the ‘amazing’ organ that is the reddish-brown liver, which weighs about three pounds and is rubbery to the touch. Sitting on the right side of the stomach with the gallbladder and parts of the pancreas and the intestines below it, the liver which is protected by the rib-cage, is the human body’s largest internal organ.
The liver consisting of the right and the left lobes, along with the gallbladder, the pancreas and the intestines, digests, absorbs and processes food, says Dr. Niriella, explaining that its main role is to filter the blood coming from the digestive tract, before passing it to the rest of the body. The liver is like the ‘engine of a car’ and contains billions of specialized cells that are linked to a well-organized system of bile ducts and blood vessels which form the biliary system.
In a nutshell, this Hepatologist gives the critical functions of the liver as:
The removal of bacteria and toxins from the blood
The prevention of infection and regulation of immune responses
The processing of nutrients, medications and hormones and the storage and production of vitamins
The production of bile, which helps the body to absorb fats, cholesterol and fat-soluble vitamins
The making of proteins that help in blood-clotting
However, certain diseases can hit this wonder organ very hard, curbing its activity and necessitating a liver transplant, MediScene learns.
 Some of these diseases are:
Some of these diseases are:
Cirrhosis – Both non-alcoholic and alcoholic which are the commonest causes of cirrhosis in the country leading to chronic liver failure. This contributes to long-term damage, bringing in its wake permanent scarring. The rare causes of cirrhosis meanwhile include chronic viral Hepatitis B and C, auto-immune hepatitis and Wilson’s disease (excess copper deposition and damage to the liver).
Acute Liver Failure – Due to viral infections such as Hepatitis A and drugs such as paracetamol overdose.
According to Dr. Niriella, a liver transplant is a surgical procedure that removes a liver that no longer functions and replaces it with a healthy liver. Transplants can be performed with a part of a healthy liver from a living donor or a full liver from a deceased donor. Living-donor liver transplants are possible as the liver regenerates and returns to its normal size after surgical removal of a part of it. The “match” in both cases should be right with regard to the blood group (the donor’s and recipient’s) and even in size. The body size correlates to the liver and as such, in a deceased donor transplant, a small liver will not be suitable for transplant in a large person.
Back in October 2011, this fascinating ability of the liver to regenerate enabled the Colombo North Hepatobiliary and Liver Transplant Unit to perform another first in Sri Lanka. In a mother-daughter donor-recipient exchange, they transplanted a part of the liver of U.K.G. Muthu Menike, 51, in Niroshani Kumari Thoragolla, 21. (The Sunday Times reported this on November 6, 2011 headlined ‘A day to remember’.)
Then and even now whether it is a living-donor or deceased-donor liver transplant, the unit gives credit to “absolute team work” with support also being extended from external institutions, making it a truly Sri Lankan effort. The other institutions they coordinate with are the National Hospital of Sri Lanka (NHSL), the National Institute for Nephrology, Dialysis and Transplantation, Maligawatte, and the Intensive Care Units (ICUs) of major state hospitals from which donor livers are offered for transplantation.
For Consultant Gastroenterological and Hepatobiliary Surgeon, Dr. Rohan Siriwardena and other Transplant Surgeons, their skills would come into play when extricating the donor-liver from all its connections, as it is joined to many parts of the body. If the liver is being brought from another institution as in the case of the first transplant in Sri Lanka for acute liver failure performed on July 20, the time such a liver has to be kept on ice would be of crucial importance before it is linked to the key structures of the recipient such as the hepatic vein, the portal vein, the hepatic artery and the bile duct.
“Blood loss,” will be the major worry for Consultant Anaesthetist Dr. Bhagya Gunetilleke who will have to anaesthetize the patient and maintain stable blood pressure, keep him/her ventilated and pain-free.
The team performed the liver transplant on Hemamali on March 9 and gradually her weight has increased from 39kg to 44kg now. The couple has come for the check-up, after offering merit to the deceased donor, a youth, because of whom Hemamali is alive today.
While her husband says that all medical advice was followed to the letter to keep infection at bay, Hemamali smilingly adds that when she got up from her sleep after the transplant, there was no pain.
The care from the whole team was incredible, she says, with her husband adding that sevaye watinakama mila karanna be (one cannot place a value on the service provided by them)………and without a cent being charged. Even the token gifts that the family brought for the team were gently declined, as for them the greatest “gift” was seeing Hemamali healthy and well again.
The medical team in addition to Dr. Niriella comprises Dr. Anuratha Kajendran, Dr. Vithiya Rishikesavan, Dr. Achini Withanachchi, Dr. Anuradha Dassanayake, Prof. Arjuna de Silva and Prof. Janaka De Silva.
The surgical team consists of Dr. Siriwardena and Dr. Suchintha Thilakaratne, working closely with NHSL’s Dr. Ruwan Dissanayake and Maligawatte’s Dr. Nalaka Gunawansa.
The anaesthetic team, meanwhile, includes Consultants Dr. Gunetilleke, Dr. Carmel Wijesekera, Dr. Nilmini Wijesuriya, Dr. Sagari Ranasinghe and Dr. Asantha De Silva along with the trainees Dr. Tharanga Gunaratna, Dr. Nadeeshya Welikala, Dr. Rachini Vithanage, Dr. Vishaka Kerner, Dr. Jeewaka Kulatissa, Dr. Roshangani Ranamuni and Dr. Thamosha De Silva.
The others who form the perfect team include the nurses, Consultant Microbiologist Dananja Karmaline; Consultant Nephrologist Dr. S. Mathu; and the Operating Theatre, Medical and Surgical ICUs, Blood Bank, laboratory and minor staff of the Colombo North Hospital.
As Hemamali protects her new liver by having a normal and healthy diet and taking the medications as prescribed, Dr. Niriella says that multiple drugs have to be taken by the liver-recipient to prevent her body from rejecting this “foreign” organ even though the matching has been spot on. Gradually, the medications will be tapered down, but she will have to be on immuno-suppressants life-long.
This is a small price that Hemamali and the others who have got new livers have to pay after their close call with death.
(The article on the transplant for acute liver failure titled ‘First-ever transplant for acute liver failure’ was published in the Sunday Times of August 13, 2017)