News
All must wage war against dengue
The “small things” matter in prevention campaigns, while a strong partnership between the authorities and the people is of vital importance in the war against the tiny mosquito that is the dealer of dengue.

Dr. Razia Pendse Pic by Priyantha Wickramaraachchi
This is the crystal clear message from the new World Health Organization (WHO) Representative to Sri Lanka, Dr. Razia Pendse, who urges a multi-sectoral and multi-pronged approach in the battle against dengue. Feedback and suggestions from the public should also be taken into account, while mobilizing them to be the foot-soldiers, guided by the grassroot-level health staff.
Just shine a torch into a pond you may have in your home or garden – the larvae of Aedes aegypti, the dengue vector, will shy away from the light and scuttle to the corner. This is the ‘torch-test’ which will show the naked eye the snake-like larvae, sensitive to light, wriggling away from the light.
This is one of many simple things Dr. Pendse, who flew into Sri Lanka just two months ago at the height of the dengue epidemic, says that people can do to spot breeding places, followed by action to rid one’s home and environments of this dealer of disease and death.
“Anyone can do the torch-test and no specialists are needed for it. Dengue is everybody’s business, not just that of the government,” she reiterates, pointing out that when looking at the numbers in Sri Lanka everyone knows somebody affected by dengue or has been hit by it themselves. Dengue, transmitted by a teeny-tiny mosquito, has become a national epidemic.
According to Dr. Pendse there is much expectation from the government including the National Dengue Control Unit, even with regard to cleaning-up houses. However, there is only so much the authorities can do. The community is not active but passive and the involvement seems low. “To make a sustainable change, all of us need to chip in.”
To win the battle against dengue, the authorities and everyone else including the private sector, civil society, non-governmental organizations, offices, schools and workplaces should work together in concerted clean-up drives, she says, explaining that these have to be supported by public health officials and fumigation teams also doing the rounds.
“No single initiative will be successful against the dengue mosquito,” is Dr. Pendse’s view, with community involvement being imperative, not just during this epidemic but all-year round to curb and keep Aedes aegypti at bay. Families and communities should be motivated to go on a different kind of “treasure hunt” weekly to “look for water containers” which could serve as ideal breeding grounds for the dengue mosquito and dispose of them in the right manner. The “prize”, of course, would be staying free of dengue in the home and the community.
The dengue mosquito’s flying range is about 400-500 metres at most. As such, it would have access to about 50 houses within a ½ to 1 km radius, the Sunday Times learns. So all dengue prevention programmes should target homes, schools, places of religious worship and shops both big and small including tyre-repair places. The willing engagement of the public for sustainable clean-up programmes is vital and people will get involved if they are made to understand that it is for their own benefit, to prevent their children getting dengue, says Dr. Pendse.
The Health Ministry, meanwhile, should guide people how to find breeding spots, how to clean-up their homes and environs and then evaluate whether these efforts have paid off. If such efforts are carried out on a Saturday, two weeks later there should be an evaluation whether a proportionate reduction of possible breeding sites is seen. This could be measured through the reduction of dengue patients being sourced in that particular area.
Therefore, a multi-pronged attack is needed, with monitoring and evaluation as an essential component, to ensure sustainability.
| People should know what to look for | |
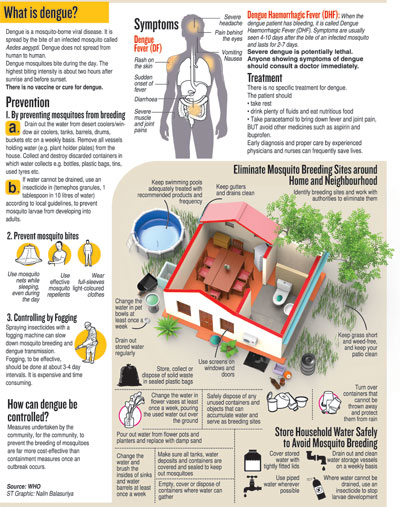
| Here is some important information that the people should know, says Dr. Razia Pendse: The dengue mosquito loves dark and dingy places, “cryptic” (hidden) sites and “unseen” spots, away from sunlight. These are the places they hide in and also lay their eggs. In a single household, there could be 18-20 breeding spots. Any container with water can turn into a breeding spot for Aedes aegypti — flower vases; tiny containers with a little water and flowers before a small shrine in the home; holy water containers in places of worship; refrigerator defrosting trays; air-conditioner outlet pipes and also tiny puddles that could form at the opening; the tray which catches the water from under a pot with a plant; the axils of such plants as aloe vera; artificial water fountains; unused toilets; and many more. Overhead water tanks and their overflow pipes, high on inaccessible roofs become an undisturbed and safe haven for mosquitoes especially during dry spells like the present. For such tanks and other large containers that are not easy to clean, Temephos/abate 1mg/litre, the effects of which last for three weeks, can be used to prevent mosquito breeding. The dengue mosquito lays eggs on the walls of the container just above the water level. The eggs do not float on the water. So even if the water is drained away from the container, the eggs can remain in dry conditions for about 400 days (more than a year) and then hatch even if a drop of water falls on them. This is why the sides of the containers or bird-baths etc., need to be scrubbed well after the water is disposed of in the first instance. It takes about seven days for the egg-larva-pupa cycle to deliver the adult mosquito. People need to be told what to look for and how to dispose of whatever is found, in the right manner. For example, if they do find containers which could retain water, just dumping them with the garbage will not be the solution Wearing long-sleeved and protective clothing. Dr. Pendse says that even though stockings cover the legs, they do not give protection from mosquito bites. Wearing a mosquito repellent If, however, anyone should experience non-specific flu-like indications such as high fever, a severe pounding headache, abdominal pain and dizziness, Dr. Pendse urges them to see a doctor immediately without “waiting it out”. “The monitoring of patients is a must. But all those with dengue do not need hospitalization. They should be monitored and if doctors so advise, family members could do that. However, for people living alone it would be important to seek help. The clinical management of dengue patients is good in Sri Lanka,” she says, adding that the capacity should percolate from major hospitals to smaller hospitals in the peripheries to reduce the patient-load at bigger centres. There is no anti-viral treatment for dengue, only the management of symptoms. Paracetamol and adequate fluids are recommended, while non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen should not be taken. NSAIDs could lead to bleeding and cause other side-effects which would complicate the clinical picture. Referring to vaccination against dengue, Dr. Pendse adds that there is one vaccine but that has not been pre-qualified by the WHO as all data have not come in with regard to its efficacy and safety. However, some countries in Asia and Latin America are using this vaccine. |
| Urgent measures needed to control this bearer of dengue | |
| Dr. Razia Pendse sketches the profile of Aedes aegypti, with its own identification ‘mark’ being ‘white-striped’ legs, and reiterates the need to control this disease-bearer. This mosquito usually bites in the day-time. Its lifespan is at least a month. It needs its full blood meal on alternate days. The mosquito gets the dengue virus when it bites a person who has dengue. After several days of getting the virus, it can transmit the virus to other people, it bites thereafter. It is an active little insect, moving from person to person, on average biting 5-7 people, to get its full blood-meal. The mosquito infected with the dengue virus can pass the virus to all of the other people it bites. This is why everyone needs to be careful. Some of these people who have got the dengue virus from the mosquito will show symptoms, while others may not (asymptomatic – not showing illness), but both groups can pass the virus to many more mosquitoes. Therefore, a single infected mosquito which would take blood-meals for 15 days in a month could easily infect about 75 people or more with dengue. This is where the danger lies – for large numbers of mosquitoes are not needed to spread the disease, a few will carry out their ‘job’ effectively, which is most unwelcome for humans. When a dengue patient is diagnosed, what should follow is shown by Dr. Pendse: Efforts are needed to identify the site of infection – was it the home, the school, the tuition class, the workplace, the construction site etc. However, those who are not ill (asymptomatic) but carrying the dengue virus cannot be discounted as they will be more mobile than those who are ill. |

