Pain, pain, go away
View(s):Many patients seek relief at the vital Pain Management Unit of the National Hospital, and the unit also conducts a clinic at the Maharagama Cancer Hospital. Kumudini Hettiarachchi reports

Ruwanmali has relief from excruciating pain now
It is something we fear immensely and we see it in the eyes of H. Ruwanmali Tharangani (32) from Gampaha.
Excruciating pain is what she fears and it is her husband, R. Premasiri, beside her bed at the Pain Management Unit of the National Hospital of Sri Lanka (NHSL), who tells us how she would scream in agony at home.
For, she is a cancer-sufferer and the malignancy has crept insidiously from her tummy to the right hip bone and onto her spine, he says, explaining that she would be hit by “uhulanna beri kekkuma” (unbearable pain).
Now, however, with medication from the Pain Management Unit there is relief for her, he says, as Ruwanmali, a mother of two children aged 10 and seven, nods in agreement.
Many are the people seeking solace from the Pain Management Unit on the 7th Floor of the Neuro-trauma Building on Monday as we walk in. Brightly but not garishly lit, just opposite the seats of the patients is a tank with gold, white and black fish swimming around, while a TV on low volume makes the men and women gathered there smile over a comedy.

A patient being examined for tenderness and backpain. Pix by M.A. Pushpa Kumara
A vital need, this Pain Management Unit opened exactly three years ago on June 21, 2013, is now headed by Consultant Anaesthetist Dr. Hemantha Kumarihamy. Her team consists of Senior Registrar Dr. Dushyanthi Jayasekera, Medical Officers Dr. Nandani Lokuliyana, Dr. Pirabaanandanan Kumarasingham and Dr. M.H.M. Nizar and Nurse-in-Charge Wajira Kumudini and Nurse Ayantha Karunathilake and three minor staff members.
More than 30 to 40 patients, mainly referred by doctors in government hospitals across the country, seek relief daily from the Pain Management Unit, while Dr. Kumarihamy and her team also visit the Maharagama Cancer Hospital once a week, MediScene learns.
“Monday, Wednesday and Friday are the clinic days at the Pain Management Unit while on Tuesday we do a ward round at the Maharagama Hospital and conduct a clinic in the afternoon there. Thursday is our procedure day when we administer injections to chronic pain-sufferers with the help of a radiographer and C-arm-guidance at the unit,” explains Dr. Kumarihamy.
Most of the patients are referred to the Pain Management Unit from neurosurgery, orthopaedic, rheumatology, surgery and plastic surgery, medical, ear-nose-and-throat (ENT) and oncology wards, we learn.
 Dr. Kumarihamy then delves into pain, explaining that it could be grouped as ‘acute’, ‘chronic’ or ‘acute on chronic’. Citing examples, she says that ‘acute’ pain would follow an injury or an operation, whereas persistent pain lasting more than three months would be ‘chronic’ pain. There would also be ‘cancer-pain’ or ‘non-cancer pain’.
Dr. Kumarihamy then delves into pain, explaining that it could be grouped as ‘acute’, ‘chronic’ or ‘acute on chronic’. Citing examples, she says that ‘acute’ pain would follow an injury or an operation, whereas persistent pain lasting more than three months would be ‘chronic’ pain. There would also be ‘cancer-pain’ or ‘non-cancer pain’.
Usually, pain can be grouped as ‘neuropathic’ (pathological) or ‘nociceptive’ (physiological).
Neuropathic pain – There is no obvious reason for this complex chronic pain. Some of the underlying causes could be nerve fibres themselves being damaged, dysfunctional or injured which in turn sends incorrect signals. There could be an increase in free nerve-endings, an increased secretion of pain-transmitting chemicals in the gap between nerves or the brain misreading the sensation of touch to be that of pain.
 Nociceptive pain – If there is a cut somewhere, the free nerve endings will get stimulated by the release of a lot of chemicals and the injury site would also get inflamed. The stimulated nerve-endings will send a signal along the nerves to the spinal cord, after which the signal would cross to the other side of the spinal cord and go to the thalamus located in the brain. In the thalamus, the cortex would get an indication of the cut-injury where there is pain; the limbic system would generate pain-associated emotions such as fear and sadness; and the brain stem linked to vital centres in the body would activate higher pulse and respiratory rates and also blood pressure. This is the ‘pain pathway’. In reverse, there is a descending pathway responsible for modulation of the pain signals. (See graphic)
Nociceptive pain – If there is a cut somewhere, the free nerve endings will get stimulated by the release of a lot of chemicals and the injury site would also get inflamed. The stimulated nerve-endings will send a signal along the nerves to the spinal cord, after which the signal would cross to the other side of the spinal cord and go to the thalamus located in the brain. In the thalamus, the cortex would get an indication of the cut-injury where there is pain; the limbic system would generate pain-associated emotions such as fear and sadness; and the brain stem linked to vital centres in the body would activate higher pulse and respiratory rates and also blood pressure. This is the ‘pain pathway’. In reverse, there is a descending pathway responsible for modulation of the pain signals. (See graphic)
“Pain differs from patient to patient,” says Dr. Kumarihamy, explaining that depending on the modulation, the final perception of pain intensity in each person will be different. It will also vary depending on the education, spirit, socio-cultural beliefs etc, of each person.
Acute pain is managed by clinicians including surgeons, anaesthetists etc., in the intensive care units and wards themselves, while chronic pain sufferers are referred to this National Pain Management Unit which is the only one for the whole island in the state hospital system.
When a patient is referred to them, as pain could be a sign of other issues, the team at the Pain Management Unit takes a detailed case-history and also several tests to rule out other diseases.

A patient being prepared for the administration of an injection under C-arm guidance
Pain, both chronic and neuropathic, comes in various forms:
Facial pain or trigeminal neuralgia – A most painful condition in which there is a sudden, severe, electric shock-like or stabbing pain lasting several seconds on the face, around the lips, eyes, scalp and forehead. It is usually unilateral, regularly affecting one-half of the face.
Backache – Including lower back, middle back or low back pain with sciatica, nerve and muscular problems, degenerative disc disease and arthritis could be the cause.
Neck-pain with radiculopathy – This could come about due to a ‘pinched nerve’ which could result from a nerve compression or irritation where it branches from the spinal cord. The pain caused by such a condition radiates into the shoulder and may also result in muscle weakness and numbness going down the arm and into the hand.
 Chronic pancreatic pain – This could be a dull or sharp pain which becomes worse after eating. Starting in the epigastric area, it could also radiate to the back. Nerve entrapment pain – This could be caused by nerves getting pinched or compressed in any part of the body.
Chronic pancreatic pain – This could be a dull or sharp pain which becomes worse after eating. Starting in the epigastric area, it could also radiate to the back. Nerve entrapment pain – This could be caused by nerves getting pinched or compressed in any part of the body.
Post-herpetic neuralgia – Due to damage caused by the varicella zoster virus, the pain is usually confined to an area of the skin, following a herpes zoster (shingles) infection at the same site. Headache – Pain anywhere in the region of the head or neck, could be due to migraines, tension-type headaches or cluster headaches.
Fibromyalgia – This is a condition in which there is muscular or musculoskeletal pain with stiffness and tenderness in a specific area. There is symmetrical distribution of the pain across the body. Pain associated with cancer – This could be caused by a tumour pressing on bones, nerves or other organs. Sometimes cancer treatment could also cause numbness, tingling or a burning sensation.
Depending on the patient’s condition, a treatment mode would be decided on – medications or injections or a mix of both.
For Dr. Kumarihamy many have been the poignant moments when patients smilingly tell her that they are pain-free but one comes to memory immediately.
It is the case of a 60-year-old woman who had tried everything due to agonizing facial pain. She had doctor-hopped and also got most of her teeth extracted thinking they were the culprits of her agony. Ten years, she had suffered and in the last stages she had not been able to eat for three days neither could she open her mouth.
When she came to the Pain Management Unit, the team had got into action – to help her overcome her disastrous experience with pain. Having diagnosed trigeminal neuralgia and put her on a regimen of injections and medications, the usual thank-yous from a grateful patient were not needed. Her smile had said it all — that the pain was gone.
The Pain Management Unit was set up due to the efforts back in 2013 of then President of the College of Anaesthesiologists of Sri Lanka, Dr. Kumudini Ranatunga, fully supported by Dr. Shirani Hapuarachchi along with the Director of the NHSL, Dr. Anil Jasinghe and the Director-General of Health Services, Dr. Palitha Mahipala.
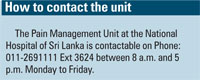
Many patients seek relief at the vital Pain Management Unit of the National Hospital, and the unit also conducts a clinic at the Maharagama Cancer Hospital. Kumudini Hettiarachchi reports.


