Learning to live with Motor Neurone Disease
It is a disease which gained much prominence after the famous English theoretical physicist, cosmologist and author Stephen Hawking was assailed by it in the prime of his youth at 21.

Stephen Hawking
Given just two years to live, he has beaten all medical predictions. He is now 74 years old having lived with this debilitating neurological disease for 53 years. With mathematics and physics being his speciality, most of his major contributions in this field have been while he continues to battle Motor Neurone Disease.
This is what should give hope to those, who like Hawking, are living with Motor Neurone Disease.
Until there is life, there is hope, is the message delivered by Senior Consultant Neurologist Dr. Padma Gunaratne attached to the National Hospital of Sri Lanka, who stresses that though there is no cure for Motor Neurone Disease, everything possible should be done to make the patient as comfortable as possible, with his/her quality of life being assured.

Dr. Padma Gunaratne
“No single reason can be attributed to Motor Neurone Disease, as it is multi-factorial,” points out Dr. Gunaratne, explaining that a person who has a genetic pre-disposition is more likely to develop the symptoms. Sometimes environmental, toxic and viral factors could also play a role.
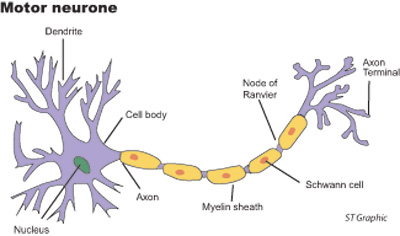
The nervous system is affected by the degeneration of motor neurones in the spinal cord and their connections to the brain known as pyramidal tracts. This causes a gradual disruption in motor activity. Motor neurones are cells that control essential voluntary muscle activity such as speaking, swallowing, breathing and walking. Usually, messages that are sent from the motor cortex of the brain through the pyramidal tracts to motor neurones in the brain stem and the spinal cord and then onto the muscles control the movement of the arms, legs, chest, face, throat and tongue, MediScene learns.
A disruption in these signals which occurs in Motor Neurone Disease would be followed by the muscles not working, gradually weakening and finally wasting away. As the disease progresses there would be uncontrollable twitching, known as ‘fasciculations’. There could also be stiffness in the limb muscles known as ‘spasticity’. Little by little atrophy sets in with weakness and muscle dissolution. During the course of the disease, the person loses the ability to control voluntary movement. Occasionally, there is also frontotemporal dementia.
“The onset is insidious and there is progressive degeneration. There is neither a cure nor a regression,” says Dr. Gunaratne, adding that the prevalence is about 4 per 100,000 worldwide. There are no studies in Sri Lanka which have determined the numbers affected by Motor Neurone Disease here. Many are afflicted by this disease in middle-age from around 30-50 years, with more men falling victim than women. The duration of the progression of the disease varies markedly from person to person and could be from about four to 20 years.
 The early symptoms include difficulty in talking and swallowing, weakness of the hands and the legs and difficulty in walking, according to Dr. Gunaratne. However, there is no numbness or pain and the cognitive (thinking, understanding, learning and remembering) functions of the brain are preserved. The control of bladder and bowels is retained and the Underscoring that when diagnosing Motor Neurone Disease, it is important to exclude all other treatable conditions, she says that the tests will include blood tests [full blood count, erythrocyte sedimentation rate (ESR), B12 levels, toxins etc] and Magnetic Resonance Imaging (MRI) of the brain. The patient needs to be screened for malignancies which should be ruled out before conclusively diagnosing Motor Neurone Disease. To confirm the diagnosis, neurophysiological (functioning of the nervous system) studies will have to be conducted in three discrete areas such as the tongue, hand and leg.
The early symptoms include difficulty in talking and swallowing, weakness of the hands and the legs and difficulty in walking, according to Dr. Gunaratne. However, there is no numbness or pain and the cognitive (thinking, understanding, learning and remembering) functions of the brain are preserved. The control of bladder and bowels is retained and the Underscoring that when diagnosing Motor Neurone Disease, it is important to exclude all other treatable conditions, she says that the tests will include blood tests [full blood count, erythrocyte sedimentation rate (ESR), B12 levels, toxins etc] and Magnetic Resonance Imaging (MRI) of the brain. The patient needs to be screened for malignancies which should be ruled out before conclusively diagnosing Motor Neurone Disease. To confirm the diagnosis, neurophysiological (functioning of the nervous system) studies will have to be conducted in three discrete areas such as the tongue, hand and leg.
Once the diagnosis is confirmed, Dr. Gunaratne says that a multi-disciplinary team consisting of a neurologist, a pulmonologist, a psychiatrist, an occupational and a speech therapist and a social service officer needs to draw up an individual care-plan for the patient. The aim will be to prolong the lifespan, while providing quality care and ensuring the quality of life. Both the patient and his family need to be counselled, with whatever resources the family has being channelled to keep the quality of life of the patient, without unnecessary spending in the hope that the patient will get cured someday. The family should essentially be involved in the management of the patient.
“As the disease progresses, the patient is not able to control his emotions. He may cry for no reason or smile for no reason,” says Dr. Gunaratne.
A close eye, meanwhile, has to be kept on the patient’s lungs and breathing, as the disease involves the respiratory muscles and there could be excessive retention of carbon dioxide (CO2). When the patient’s breathing is in jeopardy, non-invasive forms of ventilation should be resorted to. There is also the danger of aspiration when feeding. As the patient loses his ability to swallow, nutrition should be maintained through nasogastric (NG) tube or peg feeding. As there is increased salivation and drooling, suckers may have to be used.
The physical disability needs to be taken into account and the environment in his home modified according to his requirements, while the development of a form of communication with the patient is also vital. Those days pictures were used but now electronic devices come in handy. With the patient having normal cognitive functions, as the disease progresses, he may go into depression which also has to be dealt with, MediScene learns.
Dr. Gunaratne refers to the need to get a final direction or wishes from the patient about his life and assets before the patient is unable to communicate. A healthcare proxy who will ensure that the patient’s wishes are adhered to, in keeping with his culture and religion should be selected so that the patient knows that his right to make decisions with regard to his life will be honoured.
Although there is a drug – riluzole — that prolongs life from about three to 21 months, Dr. Gunaratne says that its prohibitive cost makes its use in Sri Lanka restrictive.
| Hospice urgent need There is an urgent need to establish hospice facilities for those affected by illnesses such as Motor Neurone Disease, says Dr. Padma Gunaratne, adding that then these patients would get the best care in the right environment. Many families will not be able to look after someone who is suffering from Motor Neurone Disease as with its progression the patient becomes bed-bound and needs 24-hour care, she adds. | |


