At 87 kg, he has a lot to smile about!

Before
The young couple is smiling and whispering to each other. Plans are being made to tie the nuptial knot next year. The young man is smart and the young woman pretty. This was, however, not the picture just eight months ago. The groom-to-be was 144 kilos up to November 30, last year, an unforgettable day for Anil*. That was the day his life changed forever. For, it was after November 30 that he was able to shed a heavy burden, a burden which was weighing him down from childhood.
It was the day that Anil underwent bariatric surgery through a laparoscopic or key-hole procedure. “I was chubby even as a child,” says 28-year-old Anil, explaining that he usually was the biggest boy in his class. He did try out swimming, cricket and rugby but could not continue because of his weight. A “bit overweight” when he was a teenager, the fat kept piling on and by 2008 he was 130kg, hitting the maximum 144kg, when he and his fiancée whom he had met and fallen in love with in 2012, decided it was enough.
While trying out diets to cut down on his food intake, he began going for walks. “Nothing worked,” he remembers. The research began then into the options available, with an appeal to a well-known Plastic Surgeon to perform lipo-suction on him. But the Plastic Surgeon told Anil in no uncertain terms that the fat would come back after about six-seven months and guided him in the direction of bariatric surgery to lose weight.
Picking on Consultant General Surgeon Dr. Thejana Kamil Wijeratne whom he consulted at the Asiri Surgical Hospital at Narahenpita in May 2013, a battery of tests began along with the meetings with other specialists – an Endocrinologist, a Cardiologist, an Anaesthetist, a Physician, a Dietician and a Psychiatrist.
The bariatric surgery — Laparoscopic Sleeve Gastrectomy — was fixed for November 30, before which Anil had to go on a special diet for about four weeks.
He was back at home three days after the procedure, on a liquid diet such as juices and clear soup for two weeks, a semi-solid diet of blended vegetables, cereals and fruit for six weeks and his usual diet thereafter.
Anil’s experience, soon after the bariatric procedure was a little strange. “It took me about three weeks to get used to it. I could feel that my stomach was small and whenever I ate no burps emerged,” he says, adding that he was also asked to chew his food a lot in the early days and eat only small quantities.
“Now I eat whatever I want,” smiles Anil, pointing out that the quantity is controlled automatically.
Yes, Anil is smiling, for he is now only 87kg. (*The patient’s name has been changed to protect his identity)
Dealing withthe cause rather than the symptom

After

Dr. Thejana Wijeratne
It is Consultant General Surgeon Dr. Thejana Wijeratne who delves deep into the subject of bariatric or metabolic surgery.Having undergone training in this field in Australia, before explaining the procedures of bariatric surgery, he says that deposits of fat on a person’s body, both internally and externally, are related to the food digestive (gastro – enterology) system. There is a genetic and familial component linked to this phenomenon, compounded by wrong lifestyle habits, it is learnt.
“After a certain point, it becomes driven by certain issues in the gastro-intestinal system. In bariatric surgery, we do something to the gastro-intestinal system to halt the causative factor. We deal with the cause rather than the symptom,” he says. The indications for bariatric surgery would be morbid obesity – a Body Mass Index (BMI – calculated from a person’s weight and height) of >40 or a BMI of >35 with significant obesity-related co-morbidities including diabetes, fatty liver disease, poorly-controlled or uncontrolled hypertension, high cholesterol, obstructive sleep apnoea and weight-related joint issues.
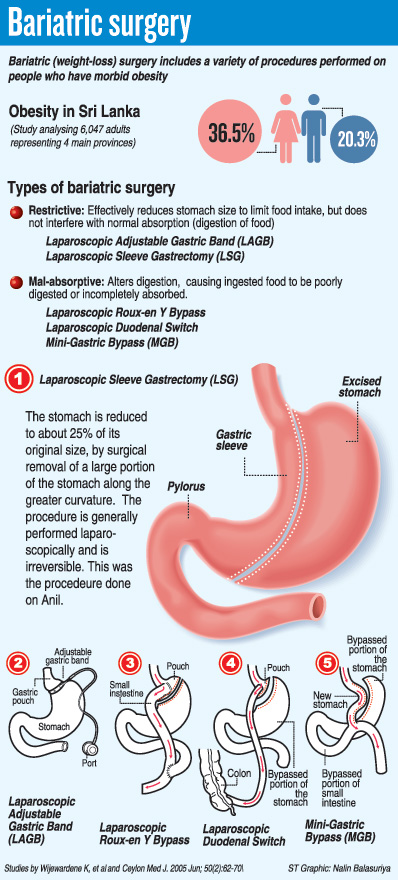
The different types of bariatric surgery or surgery for obesity are:
Restrictive bariatric surgery under which comes Laparoscopic Adjustable Gastric Band (LAGB) and Laparoscopic Sleeve Gastrectomy (LSG)
Mal-absorptive bariatric surgery under which comes Laparoscopic Roux-en Y Bypass, Laparoscopic Duodenal Switch; Mini-Gastric Bypass etc.
For Anil what was performed was a Laparoscopic Sleeve Gastrectomy (LSG), says Dr. Wijeratne, pointing out that restrictive bariatric surgery is recommended for Asians because in our dietary pattern, we put on weight due to volume-eating and volume-drinking. “Our meals consist of large volumes of high carbohydrates, in the form of heaped-up plates of rice.”
Explaining the procedure, he said that it reduced the size of Anil’s stomach and thus limited his food intake. The procedure was performed by making five or six small incisions in the abdomen, after which the laparoscope (video camera) and long instruments were inserted through them. The surgeons work with a clear view of the stomach sent to a TV screen by the video camera.
Yellows and pinks on a video screen – it was on a lazy Sunday morning in July that the MediScene team watched a bariatric procedure in the darkened 12th floor auditorium of the Asiri Surgical Hospital. It was a procedure similar to the one performed on Anil, but this time on a woman.
Pointing out that when women are obese their fertility levels drop drastically, Dr. Wijeratne underscores the fact that when their weight is reduced the ability to conceive goes up. During the Laparoscopic Sleeve Gastrectomy on Anil, about 4/5th of his stomach was taken out, leaving a narrow gastric ‘tube’ or ‘sleeve’, he said, adding that the cut is then stapled shut. This is the longest possible staple-line in any surgery.
The reduced size of the stomach limits the food intake, making the person feel full very quickly, MediScene learns. It may also decrease the person’s appetite and the amount of ‘hunger hormone’ produced by the stomach. As with any laparoscopic procedure as opposed to open surgery, wound complications are fewer, recovery is much faster and fewer pain-killers are needed, says Dr. Wijeratne. However, the risks are a leak from the staple-line. To detect this and move in fast, there has to be stringent post-procedure monitoring. The patient also needs to be committed to regular follow-ups.
Dr. Wijeratne adds that to be 100% certain that the patient’s insides are fine, they carry out a contrast-dye test 24 hours after the procedure.