A heart stopping moment
There are no ‘peaks and valleys’ – only a straight line indicates that in heart activity of 35-year-old S. Nirmala from Yakachchi in Kilinochchi has stopped.
Strangely, there is no panic or reaching out for the paddles to give Nirmala’s heart a shock to get it beating again, although the ECG (electrocardiograph which records the electrical activity of the heart) is flat on the monitor.

Nirmala recovering post-op with her mother S. Easwari by her side.
Nirmala has not gone into heart failure on the operating table of the Northern Central Hospital in Jaffna on the afternoon of July 10. Her heart has been ‘stopped’ by skilled Heart Surgeons, with the support of the anaesthetic team and the perfusion team, to repair a hole in her heart.With the ECG showing a straight line, it is time to get down to work, for the functioning of this very important organ has now been transferred to the heart-lung machine.
For me, not in the green scrubs of the surgical, perfusion, anaesthetic and nursing team, but in a grey garb with face mask and cap in place, it has been fascinating to see the ‘work’ being done on the operating table with its numerous snaking lines and pipes and monitors standing slightly away.Earlier, the anaesthetic team had put Nirmala to sleep starting their work around 2 in the afternoon, while the surgical team was having their cups of tea and pieces of butter cake. From morning Heart Surgeon and team leader, Dr. Ravi Perumalpillai has been asking whether bloods and other tests have been done.
This is the second closure of a hole in the heart within five days under open-heart surgery, the first having been done on July 6. These surgeries have been initiated by the charity, Oxonian Heart Foundation (OHF), to provide free heart surgery to needy people in the northern, eastern and north central regions of the country.
Although the Jaffna Hospital had open-heart surgery for closure of holes in the heart under hypothermic conditions, with the then Heart Surgeon leaving, the operations had halted back in the early 1980s.
In the operating theatre, as the surgical team moves in, the anaesthetic team ticks off a check-list which includes checking the name of the patient and what she is on the operating table for. Check, check, check is the motto – before anaesthesia is administered, before opening up the skin of her chest and before the patient leaves the theatre, explains an anaesthetist, adding that “this culture of safety” first permeated the oil and shipping industries, then the aviation industry and more recently the health sector.
 With ‘Time out’ being called, the surgical team then cleans up the surface area of Nirmala’s body where the surgery would take place and drapes her in surgical linen, leaving only a square patch of chest open as the ‘work area’.While the scalpel cuts open the skin, Dr. Perumalpillai urges the surgeon to “cut in the midline….stay in the middle”, after which it is time to saw open the sternum (breastbone), followed by the opening up of the pericardium (the double-walled sac containing the heart and the roots of the great vessels).
With ‘Time out’ being called, the surgical team then cleans up the surface area of Nirmala’s body where the surgery would take place and drapes her in surgical linen, leaving only a square patch of chest open as the ‘work area’.While the scalpel cuts open the skin, Dr. Perumalpillai urges the surgeon to “cut in the midline….stay in the middle”, after which it is time to saw open the sternum (breastbone), followed by the opening up of the pericardium (the double-walled sac containing the heart and the roots of the great vessels).
Nirmala’s beating and pulsating heart comes into view. A close look at the heart follows to identify key areas, followed by the insertion of a ‘pipe’ (in fact a tube) into the aorta, which is then attached to the heart-lung machine, to create a half bypass. Next the pipes go into the superior vena cava and the inferior vena cava. Tapes snug (tighten) down the pipes, so that no blood leaks from any of the vessels, before the full bypass is in place. It is then that the heart-lung machine takes over.
“Look at the difference in the colour of the blood,” says another Heart Surgeon on the team, Dr. Nihal Kulatilake, pointing to the blood being channelled into the heart-lung machine. The machine which has taken over the functioning of the heart, keeps the circulatory system in place, sending out oxygenated blood (red) all over the body and bringing in the de-oxygenated blood (blue) to the machine.
Thereafter, a cross-clamp is applied to stop the heart from beating and the cardioplegia is run, closing down the metabolic rate. It is then that the ECG indicates a straight line on the monitor. Explaining that cardioplegia means the paralysis of the heart by the infusion of a cold solution with a high potassium concentration into the coronary circulation to protect the myocardium (heart muscle) from damage and death, Dr. Perumalpillai says that the heart-lung machine has taken over the tasks of gas exchange done by the lungs and blood circulation done by the heart. When the heart is isolated, it does not receive any blood or oxygen.
Nirmala’s heart has stopped. “A true life-and-death operation,” says Dr. Kulatilake. Slowly and steadily, the atrium is then opened up and the hole repaired, taking a patch of the pericardium from the patient itself, which ensures that there is no risk of rejection as it is not a foreign body. The reverse process takes place thereafter, with the closure of the atrium, taking the clamp off, weaning the patient off the heart-lung machine and restoring the beating of the heart.
Before closure of the chest, meticulously, the nurses not only have to count each and every instrument used in the surgery but also every single swab and mark on a white board prominently displayed on the wall to ascertain that nothing has been left behind inside the patient. And the ECG line begins its peaks and valleys ‘sketch’ across the monitor indicating that the heart is back to normal. “The heart looks good,” says Dr. Kulatilake, relieving the slight tension build-up in the operating theatre.
For the team, it’s all in a day’s work.
Dr. Nagaratnam Sriskantharajah, Dr. Ravi Perumalpillai and Dr. Nihal Kulatilake comprised the surgical team; Kamal Gunasekera and Pratheesh Maheswaran, the perfusion team; and Dr. Sundaralingam Premakrishna and Dr. Arulmoli Janaki and Nurses Ramachandran Neruka and Mayoori Theepan, the anaesthetic team.
The theatre team included Nurses Vijeyabaskaran Vimalathevi and Ariot Sivasubramaniam, while the team from Oxford which facilitated the surgery consisted of Consultant Anaesthetist Dr. David Pigott, Specialist Registrar in Cardiothoracic Surgery, Dr. Sajiram Sarvananthan, Theatre Sister Angela Grantham, Anaesthetic Sister Louise Wilkins and ICU Sisters Shirley Janus and Wendy Allen.
How a hole in the heart is detected
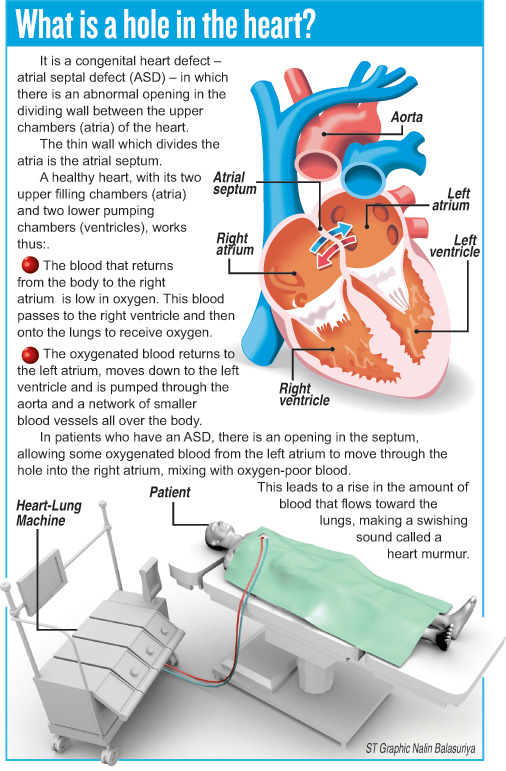
It is the swishing sound called a heart murmur, which enables Cardiologists to detect a hole in the heart. When a murmur is heard, other tests including a chest X-ray, an ECG and an echocardiogram (echo) will follow. The ECG would indicate the volume overload of the heart’s right side and the echo produces a picture of the heart, through sound waves, which can show blood flow through the heart chambers.
More girls than boys have ASDs. They occur during foetal development and are present at birth. Depending on the ASD’s size and site, the symptoms would differ. While most may not have symptoms, those with large holes in the heart may present with poor appetite, poor growth, fatigue, shortness of breath and lung problems and infections including pneumonia.
In patients with very small ASDs, they may close on their own but larger ASDs need treatment. While some can be closed in a cardiac catheterization lab, others may require open-heart surgery. Under cardiac catheterization, a thin, flexible tube or catheter is inserted into a blood vessel in the leg that leads to the heart and a special implant positioned into the hole, sealing it. However, in the case of Nirmala, it was open-heart surgery to fix the hole.


