Neuro and Spinal Surgeon
Strangely though, the Neurosurgeon is asking the patient to raise his arm, say something or write a word or two and he is doing just that.This is how Neuro and Spinal Surgeon Dr. K. Sridhar performs brain surgery on some of his patients at the Global Hospitals and Health City in Chennai, India.
It is ‘Awake Craniotomy’ that Dr. Sridhar who was in Sri Lanka in early April discusses with MediScene, when we meet him on April 3 in Colombo.
Reiterating that in tumour removal from the brain, not only does the Neurosurgeon try to excise it completely but he also has to prevent the patient from suffering a disability due to the surgery.
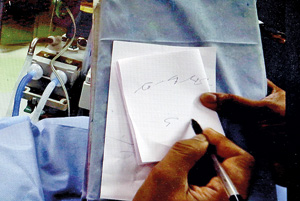
The patient is asked to write during the procedure
‘Awake Craniotomy’ comes in handy for lesions and tumours in ‘eloquent’ or crucial areas of the brain which control speech or hand and leg movement. Till recently these areas were thought to be untouchable as surgery could leave in its wake a major disability, MediScene learns.Having performed about 30 ‘Awake Craniotomies’ in the past two years, Dr. Sridhar who is Director of the Institute of Neurosciences and Spinal Disorders and Chief Brain and Spine Surgeon of Global Hospitals and Health City is quick to point out that this procedure cannot be performed on all patients. The patient has to be in the right of frame of mind to undergo such a procedure.
“It must be a person who is very cooperative who would not get scared when suddenly he wakes up in the operating theatre, with his head open, with all sorts of scary sounds around him,” says Dr. Sridhar, pointing out that patients are heavily counselled by the surgical and anaesthetist team before they decide one way or another. “The anxious ones are not suitable for this type of procedure.”
The surgical team too should not be rushing around the operating theatre (OT) during this procedure as it would cause anxiety in the patient. “In fact, even outside our OTs there is a board which states: ‘Awake Craniotomy — silence please’, because we don’t want anything to upset the patient,” he says.Usually deployed for the removal of tumours, this procedure is now being used for epileptic patients, MediScene learns.
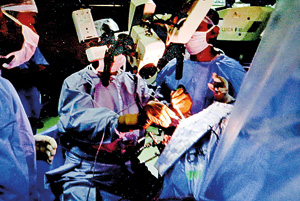
Dr. Sridhar performing 'Awake Craniotomy'
Explaining that during the ‘Awake Craniotomy’ procedure there are lots of ‘adjuncts’ to help them, he picks out Functional Magnetic Resonance Imaging (fMRI) which would clearly show the patient’s brain areas which are linked to speech and motor skills (movement of hands and legs).“When you get the patient to talk or move his/her hands or legs that area will light up on the MRI,” he says.
He delves deep into the brain — there are brain cells which send their fibres down to the spinal cord and it’s crucial that we don’t destroy either the nerve cells or the fibres during the procedure, he points out. This makes it vital for us to see how the fibres are located in relation to the tumour as well as their pathway to the spinal cord. The “adjunct” which maps the fibre tracks is Diffusion tensor Imaging (DTI) or Tractography, according to him.
If the tumour is located close to the ‘speech area’ in the brain and the fibres are very close, then we can decide from which direction we should approach the tumour, the trajectory, so that the patient is relatively safe, he says. A lesson on the all-important organ — the brain – follows, before getting into the nitty-gritty of ‘Awake Craniotomy’. The brain itself does not feel any pain sensation, explains Dr. Sridhar. It is pain-free. What feels the pain are the scalp, the bone and the coverings of the brain.
During the procedure, the patient is sedated and put into deep sleep by the Anaesthetist who has to provide the right balance of analgesia (pain relief) and sedation. The patient’s head is fitted into a frame and a skin flap is opened up followed by scalp or bone flap, being removed with a craniotomy cutter which is a high-speed drill. This is after the administration of a local anaesthetic as a scalp-block.
As the depth of sedation is important throughout the procedure, the patient’s brain activity needs to be monitored. The entropy processes such as how deep asleep the patient is are monitored through an EEG which transmits information to a monitor. When we are ready to excise (cut out) the tumour, the Anaesthetist titrates the sedation, reducing the drug to make the patient wake up gradually.
Brain surgery is performed using an operating microscope which allows Dr. Sridhar to visualise the normal and tumour tissues clearly, making the surgery precise to the millimetre. When asked why the patient should be kept awake, Dr. Sridhar’s simple explanation is that when the patient is not under anaesthesia and able to communicate with the Neurosurgeon, the information is ‘live’. Otherwise, intra-operative monitoring and cortical stimulation would give only “static” knowledge and we don’t know what is happening.
Under this procedure, we can ask the patient to raise the hand or talk to us, he says, citing the case of a 45-year-old accountant we see on video talking to Dr. Sridhar in Hindi and Bengali. “I’m asking him to do things and he’s doing them. He’s asking me whether the operation is going well.”
The Neurosurgeon-patient interaction is especially important when the excision of the margins of the tumour where it connects up with normal brain tissue is being done. When the patient is awake we know how far we can go without harming him and it allows the maximal excision of the tumour, says Dr. Sridhar, adding that then a change in the technique may be used.
With fMRI guidance when we know that we are getting close to a critical area of the brain, we get him to write, he says, adding that towards the end of the surgery they are then sure that all functions are intact. The accountant wanted to see the tumour and I showed it to him, says Dr. Sridhar, adding that an 80-year-old woman had a drink of water during her head surgery because she was thirsty.

Dr. K. Sridhar
The most poignant case, though, for this Brain Surgeon is the young man who was working in the Middle East and came back to India to look for a bride. What he found was a tumour in his brain, he says, adding that although it was not highly malignant, the glioma, had to be taken out. He did undergo ‘Awake Craniotomy’ 2½ years ago. Dr. Sridhar has asked him to wait another two years before tying the knot.
Once the tumour is removed, the patient’s sedation is increased before the wound is closed, it is learnt. The only thought throughout the ‘Awake Craniotomy’ procedure that fills the mind of Dr. Sridhar and guides his skilled hands is that he cannot let the patient down. Having the patient wide awake is of great help and assurance as the surgical team knows that he/she is fine and would not come out of the OT with paralysis or speech problems.
Dr. Sridhar’s visit was facilitated by the Sri Lankan country office of the Global Hospitals Group, India, Forte Pharmaceuticals Pvt. Ltd. This eminent Brain and Spine Surgeon had held discussions at the Peradeniya Medical Faculty, the Kandy Society of Medicine and the Colombo South Teaching Hospital in Kalubowila.


