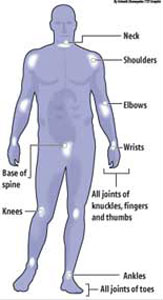
How to deal with psoriatic arthritisIn this two-part article, Consultant Rheumatologist Dr. Kaleel Cassim answers questions commonly asked by people who have psoriatic arthritis. What is psoriatic arthritis? Psoriatic arthritis causes inflammation in and around the joints, usually in people who already have the skin condition, psoriasis. Sometimes, however, the arthritis develops before the psoriasis. There are 78 major joints in the body and psoriatic arthritis can affect any one of these. However, certain joints are more likely to be affected - these are shown in the Figure.
Sometimes psoriatic arthritis affects just one or two joints such as a knee or ankle, but often several joints, both large and small and on both sides of the body are involved. About a third of people with psoriatic arthritis also have a painful, stiff back or neck caused by inflammation in the spine. This is called spondylitis. Psoriasis can affect the nails with pitting, discoloration and thickening. Sometimes the joint at the end of the finger or toe can also be inflamed. There can be a sausage-like swelling of a finger or toe with psoriatic arthritis. This is called dactylitis and is caused by inflammation occurring simultaneously in joints and tendons. Painful heels can be caused by inflammation where gristle attaches to bone. Psoriatic arthritis usually affects adults but occasionally children can develop the disease. How does the rheumatologist diagnose psoriatic arthritis? Psoriatic arthritis is diagnosed based on one’s symptoms and on what the rheumatologist finds when he examines the patient. There is no specific test for psoriatic arthritis. Most rheumatologists would check for psoriasis, or a history of psoriasis in a close relative, together with arthritis and inflammation in at least one joint. It can be difficult to distinguish between psoriatic arthritis and rheumatoid arthritis. If several joints are affected rheumatologists will consider features such as the pattern of arthritis (which joints are affected) and other symptoms to distinguish between the two conditions. Blood tests for rheumatoid factor, if negative, may also help to rule out rheumatoid arthritis. Can psoriatic arthritis attack other organs of the body? Usually, apart from the skin, nails and joints, no other major organs are affected. People with psoriatic arthritis may be more likely to develop an itchy, red eye due to conjunctivitis, and some people may occasionally develop a painful, red eye caused by inflammation around the pupil of the eye. This is called iritis or uveitis. Some people may also develop anaemia (a shortage of red blood cells). Although this is not a specific feature of psoriatic arthritis it can sometimes happen as a result of long-term inflammation. How common is psoriatic arthritis? About 1 in 50 people have psoriasis, and of these about 1 in 14 will develop psoriatic arthritis. People with psoriasis may also have other forms of arthritis, such as osteoarthritis or rheumatoid arthritis, but these are not linked to the psoriasis. What is the cause? At present, the exact cause is unknown. A particular combination of genes makes some people more likely to get psoriasis and psoriatic arthritis.
Current research suggests that something (perhaps an infection) acts as a trigger in people who are susceptible to this type of arthritis because of their genetic make-up. No specific infection has been found and it may be that a variety of infections (including bacteria that live in patches of psoriasis) can trigger the disease. Will my children develop psoriatic arthritis? Your children will be more likely than the next person to get psoriatic arthritis but the risk is still low. Both psoriasis and psoriatic arthritis occur more frequently in some families than in others. Sometimes other diseases such as inflammation of the bowel (Crohn's disease and ulcerative colitis), stiffening of the spine (ankylosing spondylitis) and severe eye inflammation (iritis or uveitis) also run in the same family. The link is genetic but the risk of passing it on is low. What links the skin and the joints in psoriatic arthritis? The link is probably genetic but fortunately many treatments help both the skin and the joints at the same time. Some people find that when their psoriasis is bad their arthritis is also bad and as one improves, so does the other. It is possible that bacteria in the skin disease trigger the inflammation in the joints. Most people develop psoriasis before the arthritis but about 1 in 10 develop the arthritis first. How is it treated ? This should include the treatment of the skin as well as the joints and many patients are also under the care of a dermatologist. Initial treatment is with a class of drugs called the NSAIDs (Non-steroidal anti-inflammatory drugs). In patients who have persistent joint pain and damage another class of drugs called the DMARDs are added on. What are non-steroidal anti-inflammatory drugs (NSAIDs)? Anti-inflammatory drugs act by blocking the inflammation which occurs in the lining of your joints. They can be very effective in controlling the pain and stiffness of arthritis. Usually you will feel a benefit within hours of taking these drugs but the effect will only last for a few hours, so the tablets have to be taken at regular intervals for the benefit to continue. Some people find that these tablets are of little help, while others find that they help at first but the benefit begins to wear off after a few weeks. In this situation it sometimes helps to try a different NSAID - there are over forty available. Examples of anti-inflammatory drugs Older drugs: diclofenac, ibuprofen, indometacin, naproxen, nabumetone, etodolac, piroxicam. The main side-effect of the older NSAIDs is indigestion and, in some cases, the drugs can cause a stomach ulcer. For this reason rheumatologists recommend taking these tablets with or after food. You must tell your rheumatologist if you get indigestion while taking these drugs as something can be done to help this - some doctors prescribe drugs known as proton pump inhibitors alongside standard NSAIDs to help reduce the side-effects on the stomach. The COX-2-specific NSAIDs (see above) cause less indigestion but have other important side-effects such as increasing the risk of heart attack and stroke (there may even be a slightly increased risk of this sort with the older NSAIDs - research on this is still underway). All NSAIDs can cause side-effects including fluid retention, rashes and headache and, if you have asthma, they can make this worse. Please see next issue for part 11 of the article..........! |
|| Front
Page | News | Editorial | Columns | Sports | Plus | Financial
Times | International | Mirror | TV
Times | Funday
Times | Medi Scene || |
| |
Reproduction of articles permitted when used without any alterations to contents and the source. |
© Copyright
2007 | Wijeya
Newspapers Ltd.Colombo. Sri Lanka. All Rights Reserved. |